Neuro-Oncology Fellowship
The University of Virginia Neuro-Oncology Center

The University of Virginia Cancer Center is a National Cancer Institute-designated Comprehensive Cancer Center, at the forefront of cancer research, prevention, detection and treatment. The University of Virginia Neuro-Oncology Center was created in 2002 and is an interdisciplinary effort with Neurology, Neurological Surgery, Neuropathology, Radiation Oncology, and Neuroradiology participation. The Center is a leader in primary brain tumor clinical trials and played an important role in the approvals of bevacizumab and the Optune device for glioblastoma as well as the use of rituximab in primary central nervous system (CNS) lymphoma. Additional subspecialty clinics focus on CNS metastatic disease, the phakomatoses, and pediatric brain tumors.

The Neuro-Oncology Center has a wide geographic referral base and sees more than 500 new cases yearly. Clinicians work closely with several brain tumor translational research labs investigating microRNA, signal transduction inhibitors, immunotherapy, and brain tumor animal models. The University of Virginia Cancer Center is a National Cancer Institute-designated cancer center, being in the forefront in cancer research, prevention, detection and treatment.
Fellowship Overview
 The University of Virginia Neuro-Oncology Fellowship Program strives to provide fellows with the quality educational experience that will enable them to deliver specialized patient care in the treatment of neoplastic disorders affecting the nervous system.
The University of Virginia Neuro-Oncology Fellowship Program strives to provide fellows with the quality educational experience that will enable them to deliver specialized patient care in the treatment of neoplastic disorders affecting the nervous system.
In accordance with the United Council for Neurological Subspecialties (UCNS) and the American Board of Psychiatry and Neurology (ABPN) training requirements, fellowship education focuses on enhancing trainees’ competence in diagnosing, treating and caring for patients with a vast array of primary or metastatic central and peripheral nervous system neoplasms and any other disorders or complications affecting the nervous system that result directly or indirectly from nervous system or systemic neoplasm or from related treatment. In addition, fellows are trained and engaged in scholar activities including research, quality improvement efforts, and education of other health professionals and the public.
To further the mission of the University of Virginia Health System, Neuro-Oncology fellows are encouraged to cultivate and sustain an environment of excellence, innovation and superlative quality in the care of patients, and the creation and sharing of health knowledge within a culture that promotes equity, diversity and inclusiveness. At the completion of the fellowship training, fellows are expected to competently attend to the diagnosis and management of neurological disorders associated with cancer and its treatment at all ages of life.
Eligibility
Length of Program: 2 years
Applicants must be a diplomate in good standing of the American Board of Medical Specialties (ABMS), American Osteopathic Association (AOA), or the Royal College of Physicians and Surgeons (RCPSC) in neurology, child neurology, neurological surgery, internal medicine and medical oncology, pediatrics and pediatric hematology-oncology, or radiation oncology.
Applications
The UVA Neuro-Oncology Fellowship participates in the San Francisco Match. Please submit applications between November and January.
Foreign Medical Graduates
Foreign medical graduates with equivalent qualifications are also eligible to apply. They must have completed all three of the USMLE examinations and hold a valid ECFMG certificate.
For any other questions, please contact the program.
Program Director: David Schiff, M.D.
Program Coordinator: Keeley McNamara, (434) 982-3839
For Applicants | Graduate Medical Education
Training and Assignment Overview
Training in neuro-oncology encompasses two years of training. The first year of training focuses on gaining clinical experience in all aspects of neuro-oncology. Fellows are expected to learn the principles of biology, neuropathology, neuroradiology, neuro-ophthalmology, psychiatry, rehabilitation, neurological surgery, radiation oncology, palliative care, and the basic neurosciences as they relate to neuro-oncology. The program curriculum includes both inpatient and outpatient patient care responsibilities. The second year of training is designed to advance the fellow’s competency and independence in clinical practice, while focusing on scholarly and academic activities.
The training curriculum is designed to provide fellows with progressive responsibility for: 1) the management of patients with neuro-oncologic illness, including; 2) the evaluation and management of patients requiring medical, surgical, and/or radiation treatment; and 3) the consultation service to the medical, surgical, and radiation oncology services.

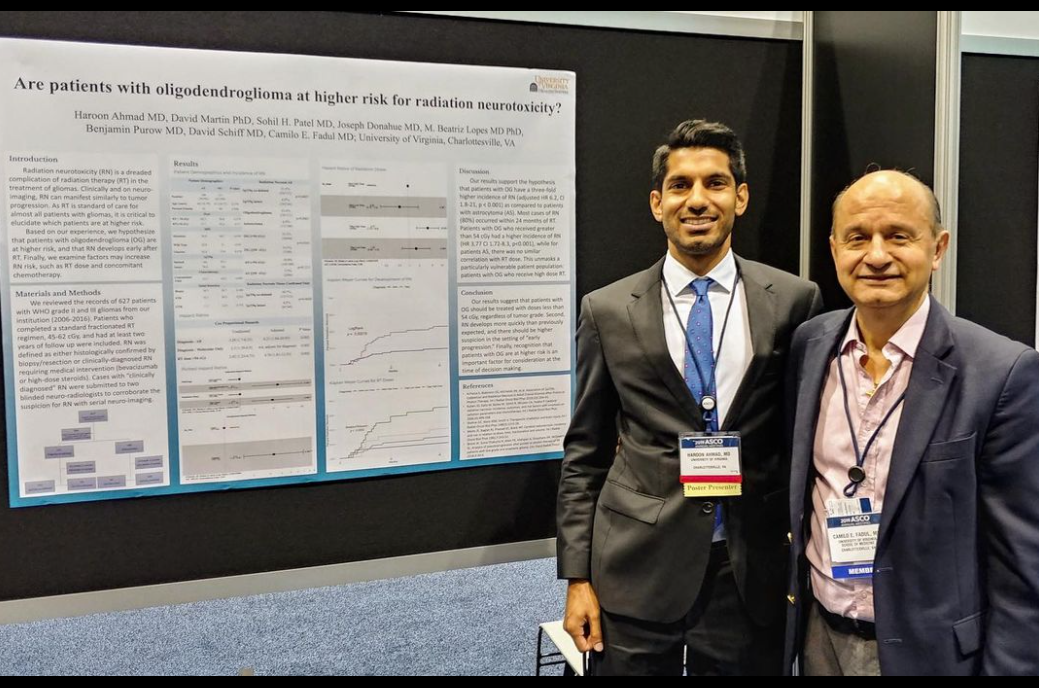
Basic Science and Clinical Research Opportunities
Fellows are provided protected time to do to do clinical and basic science research. They can gain experience in basic and translational research in one of the neuro-oncology- focused laboratories at UVA. There are ample of opportunities on participating in the design, implementation, and completion of clinical trials.
Neuro-Oncology Clinical Trials

