Featured Publications
Fast leave-one-cluster-out cross-validation using clustered network information criterion
Qiu J, Lake DE, Chernyavskiy P, Henry TR. Fast leave-one-cluster-out cross-validation using clustered network information criterion. Statistical Methods in Medical Research. 2025;0(0). doi:10.1177/09622802251345486
Spaeder MC, Lee L, Miller C, Keim-Malpass J, Harmon WG, Kausch SL. Incidence of cardiac arrest following implementation of a predictive analytics display in a pediatric intensive care unit. Resusc Plus. 2025 Jan 2;21:100862. doi: 10.1016/j.resplu.2024.100862. PMID: 39885978; PMCID: PMC11780126.
More than 90% of in-hospital cardiac arrests involving children occur in an intensive care unit (ICU) with less than half surviving to discharge. in this study, we sought to assess the association of the display of risk scores of cardiovascular and respiratory instability with the incidence of cardiac arrest in a pediatric ICU.
Qiu J, Di Fiore JM, Krishnamurthi N, Indic P, Carroll JL, Claure N, Kemp JS, Dennery PA, Ambalavanan N, Weese-Mayer DE, Hibbs AM, Martin RJ, Bancalari E, Hamvas A, Moorman JR, Lake DE, Pre-Vent Investigators. Physiol Meas. 2024 Jun 3;45(5):055025. doi: 10.1088/1361-6579/ad4e91. PMID: 38772400; PMC11485323.
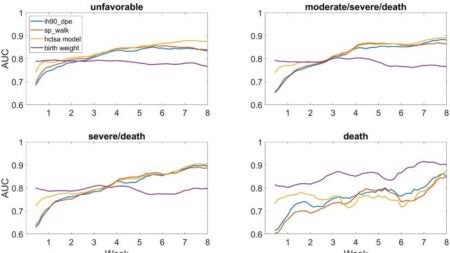
Highly comparative time series analysis (HCTSA) is a novel approach involving massive feature extraction using publicly available code from many disciplines. The Prematurity-Related Ventilatory Control (Pre-Vent) observational multicenter prospective study collected bedside monitor data from > 700 extremely preterm infants to identify physiologic features that predict respiratory outcomes.
Kausch SL, Lake DE, Di Fiore JM, Weese-Mayer DE, Claure N, Ambalavanan N, Vesoulis ZA, Fairchild KD, Dennery PA, Hibbs AM, Martin RJ, Indic P, Travers CP, Bancalari E, Hamvas A, Kemp JS, Carroll JL, Moorman JR, Sullivan BA; Prematurity-Related Ventilatory Control (Pre-Vent) Investigators. J Pediatr. 2024 Aug;271:114042. doi: 10.1016/j.jpeds.2024.114042. PMID: 38570031
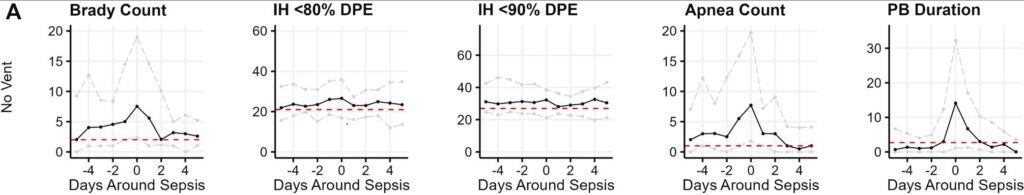
We examined the association of cardiorespiratory events, including apnea, periodic breathing, intermittent hypoxemia (IH), and bradycardia, with late-onset sepsis for extremely preterm infants (<29 weeks of gestational age) on vs off invasive mechanical ventilation.
Keim-Malpass J, Moorman LP, Moorman JR, Hamil S, Yousefvand G, Monfredi OJ, Ratcliffe SJ, Krahn KN, Jones MK, Clark MT, Bourque JM. Physiol Meas. 2024 Jun 5;45(6). doi: 10.1088/1361-6579/ad4e90. PMID: 38772399.
Kausch SL, Brandberg JG, Qiu J, Panda A, Binai A, Isler J, Sahni R, Vesoulis ZA, Moorman JR, Fairchild KD, Lake DE, Sullivan BA. Pediatric Research 2023. doi: 10.1038/s41390-022-02444-7. PMID: 36593281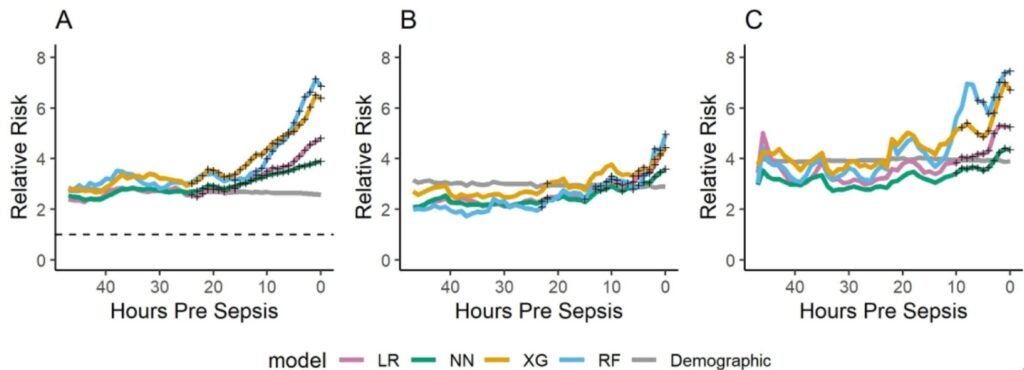
We analyzed cardiorespiratory data from very low birth weight infants admitted to three NICUs using four machine learning models we developed and externally validated to predict late-onset sepsis. We compared feature importance, discrimination, calibration, and dynamic predictions across models and cohorts.
Impact of race on heart rate characteristics monitoring in very low birth weight infants.
Sullivan BA, Hochheimer CJ, Chernyavskiy P, King WE, Fairchild KD. Pediatric Research 2023. doi: 10.1038/s41390-023-02470-z. PMID: 36650306
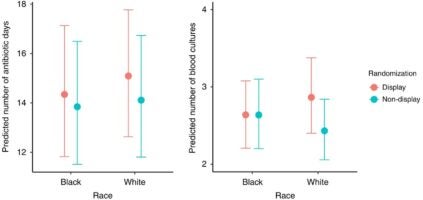
We aimed to assess whether HRCi display had a differential impact for Black versus White infants by performing secondary data analysis of Black and White infants enrolled in the HeRO RCT and evaluated the predictive performance of the HRCi for infants with Black or White maternal race.
Formanack A, Doshi A, Valdez R, Williams I, Moorman JR, Chernyavskiy P. J Gen Intern Med. 2023 Sep;38(12):2686-2694. doi: 10.1007/s11606-023-08062-1. Mar 27. PMID: 36973572
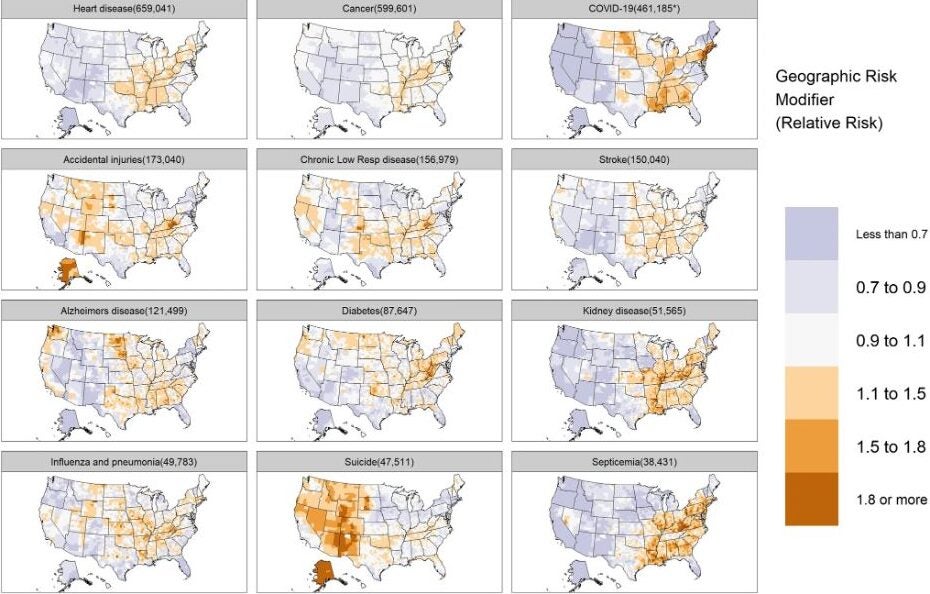
We disarticulated the associations of race, socioeconomic class, and place with risk of cause-specific death in the US through the retrospective analysis of death certificate data and application of Bayesian regression models.
Heart rate patterns predicting cerebral palsy in preterm infants
Letzkus L, Picavia R, Lyons G, Brandberg J, Qiu J, Kausch S, Lake D, Fairchild K. Pediatr Res. 2023 Oct 27. doi: 10.1038/s41390-023-02853-2. PMID: 37891365.
We previously used highly comparative time series analysis (HCTSA) to identify HR patterns predicting mortality among patients in the neonatal intensive care unit (NICU) and now use this methodology to discover patterns predicting cerebral palsy (CP) in preterm infants.
Maturation of cardioventilatory physiological trajectories in extremely preterm infants.
Weese-Mayer DE, Di Fiore JM, Lake DE, Hibbs AM, Claure N, Qiu J, Ambalavanan N, Bancalari E, Kemp JS, Zimmet AM, Carroll JL, Martin RJ, Krahn KN, Hamvas A, Ratcliffe SJ, Krishnamurthi N, Indic P, Dormishian A, Dennery PA, Moorman JR; Prematurity-Related Ventilatory Control (Pre-Vent) Investigators. Pediatr Res. 2023 Oct 19. doi: 10.1038/s41390-023-02839-0. PMID: 37857848
We characterized physiologic growth curves of apnea, periodic breathing, intermittent hypoxemia, and bradycardia in extremely preterm infants during the first few months of life using a novel sharing analytics software in the Pre-Vent observational multicenter prospective cohort study. We found that the postnatal trajectory of ventilatory control depends on the type of event, race, sex and use of mechanical ventilation.
Cardiorespiratory Monitoring Data to Predict Respiratory Outcomes in Extremely Preterm Infants.
Ambalavanan N, Weese-Mayer DE, Hibbs AM, Claure N, Carroll JL, Moorman JR, Bancalari E, Hamvas A, Martin RJ, Di Fiore JM, Indic P, Kemp JS, Dormishian A, Krahn KN, Qiu J, Dennery PA, Ratcliffe SJ, Troendle JF, Lake DE; Prematurity-related Ventilatory Control (Pre-Vent) Investigators. Am J Respir Crit Care Med. 2023 Jul 1;208(1):79-97. doi: 10.1164/rccm.202210-1971OC. PMID: 37219236
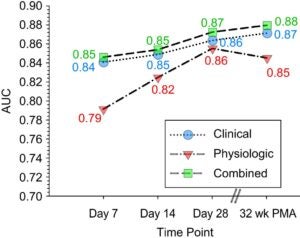
We determined that analysis of physiological cardiorespiratory monitoring data adds to prediction of unfavorable respiratory outcomes in extremely pre-term infants through the evaluation of the Pre-Vent observational multicenter prospective cohort study.
Qiu J, Zimmet AN, Bell TD, Gadrey S, Brandberg J, Maldonado S, Zimmet AM, Ratcliffe S, Chernyavskiy P, Moorman JR, Clermont G, Henry TR, Nguyen NR, Moore CC. Clin Infect Dis. 2023 Oct 27:ciad662. doi: 10.1093/cid/ciad662. PMID: 37889515
We analyzed univariate risks and developed multivariable models of BSI with 27 clinical variables from adult intensive care unit (ICU) patients at the University of Virginia and the University of Pittsburgh are responses to BSI in critically ill transplant and non-transplant recipients, and to modify systemic inflammatory response syndrome (SIRS) criteria for transplant recipients.
Spaeder M, Moorman JR, Moorman LP, Adu-Darko MA, Keim-Malpass J, Lake DE, Clark MT. Frontiers in Pediatrics. 2022. 10:1016269. doi: 10.3389/fped.2022.1016269. PMID: 24075272
We tested the hypothesis that subtle signatures of illness are present in physiological and biochemical time series of PICU patients in the early stages of respiratory decompensation using a random forest model to identify patients at risk for requiring unplanned decompensation.
Artificial and human intelligence for early identification of neonatal sepsis.
Sullivan BA, Kausch SL, Fairchild KD. Pediatric Research 2022. doi: 10.1038/s41390-022-02274-7. PMID: 36127407
We review highlights in the application of AI in neonatal sepsis prediction, describe issues of clinical prediction model developments, and review methods, considerations, and literature on neonatal sepsis model development and validation.
Kumar RS, Otero NA, Abubakar MO, Elliott MR, Wiggins JY, Sharif MM, Sullivan BA, Fairchild KD. Am J Perinatology 2022. doi: 10.1055/a-1715-3727. PMID: 34875699
We aimed to develop a framework to systematically consider signs potentially indicating sepsis in infants with very low birth weight (VLBW) by developing easy-recall acronyms for ten signs of sepsis in VLBW infants. We analyzed associations between survey data, hourly heart rate characteristic data, and the workup diagnosis grouped as culture-positive sepsis, clinical sepsis, or sepsis ruled out.
Vital signs as physiomarkers of neonatal sepsis.
Sullivan BA, Fairchild KD. Pediatric Research 2022. doi: 10.1038/s41390-021-01709-x. PMID: 34493832
We review the mechanisms of vital sign changes in neonatal sepsis, including the cholinergic anti-inflammatory pathway mediated by the vagus nerve, and the clinical implications of these changes, including their use in early warning scores and systems to direct clinicians to the bedside of infants with physiologic changes that might be due to sepsis.
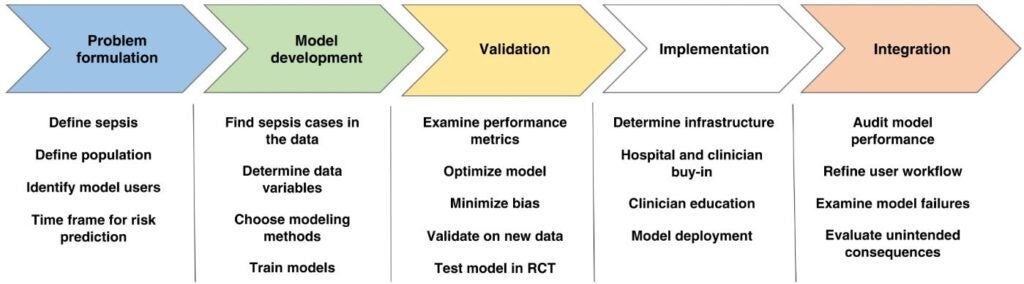
Moorman JR. npj Digital Medicine 2022. https://doi.org/10.1038/s41746-022-00584-y
We review the history of the field, beginning with heart rate variability analyses in infants in 1994 up to the present day, emphasizing the need for clinical fit, face validity, signatures of illness, mathematical foundations, ground truth events, dynamicity of predictions, and clinical trials.
Monfredi OJ, Andris RT, Lake DE, Moorman JR. Physiological Measurement 2022. doi: 10.1088/1361-6579/aca878. PMID: 36595313
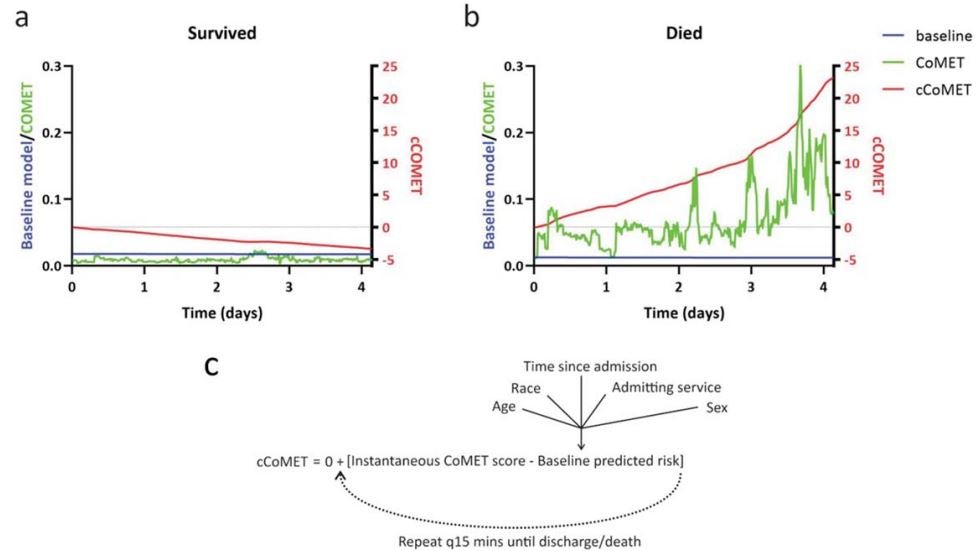
We show that higher cCoMET scores predict mortality but not length of stay, and that higher baseline CoMET scores predict higher cCoMET scores at discharge/death.
Horton WB, Hannah EE, Morales FL, Chaney CR, Krahn KN, Chernyavskiy P, Clark MT, Moorman JR. Critical Care Medicine 2023. 51:136-140. doi: 10.1097/CCM.0000000000005713. PMID: 36519987

We quantify the accuracy of clinical events associated with a risk alert threshold for impending hypoglycemia during ICU admissions from June 2020 through April 2021, using real-world testing of our validated predictive model as a clinical decision-support tool for ICU hypoglycemia.
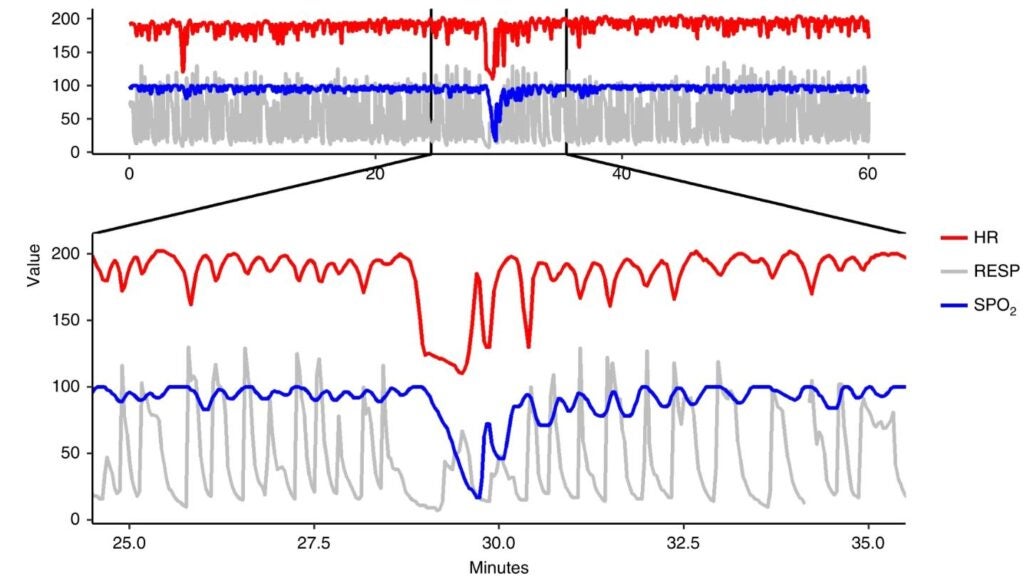
Monfredi OJ, Moore CC, Sullivan BA, Keim-Malpass J, Fairchild KD, Loftus TJ, Bihorac A, Krahn KN, Dubrawski A, Lake DE, Moorman JR, Clermont G. J ECG 2023. 76:35-38. doi: 10.1016/j.jelectrocard.2022.10.011. PMID: 36434848
We review evidence that supports the role of continuous cardiorespiratory monitoring in predictive analytics monitoring tools, specifically ECG monitoring.
Analysis of respiratory kinematics: a method to characterize breaths from motion signals.
Ashe WB, Innis SE, Shanno JN, Hochheimer CJ, Williams RD, Ratcliffe SJ, Moorman JR, Gadrey SM. Physiological Measurement 2022. PMID: 35045405 DOI: 10.1088/1361-65e79/ac4d1a
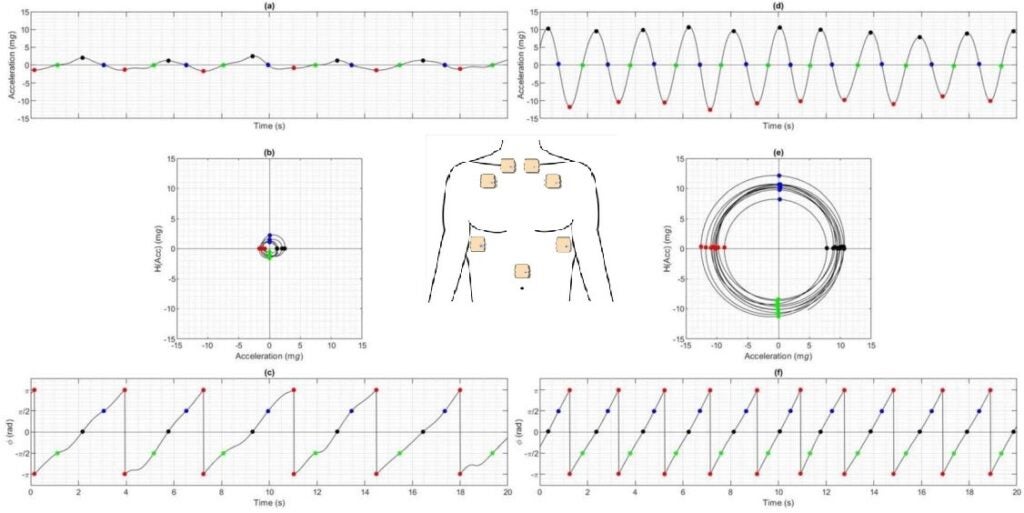
We developed numerical methods for characterizing clinically significant breathing motion patterns on a breath-by-breath basis and evaluated the relationship between respiratory kinematics and flow.
Ideal algorithms in health care: explainable, dynamic, precise, autonomous, fair, and reproducible.
Loftus TJ, Tighe PT, Ozrazgat-Baslanti T, Davis JP, Ruppert MM, Ren Y, Shickel B, Kamaleswaran R, Hogan WR, Moorman JR, Upchurch GR, Rashidi P, Bihorac A. LOS Digital Health 2022. doi: 10.1371/journal.pdig.0000006. PMID: 36532301
We propose a framework for an ideal algorithms checklist, including explainable, dynamic, precise, autonomous, fair, and reproducible, to apply it to highly cited algorithms.
Niestroy J, Levinson MA, Al Manir S, Clark TW, Moorman JR, Fairchild KD, Lake DE. npj Digital Medicine, 2022 DOI: 10.1038/s41746-021-00551-z. PMID: 35039624
We applied highly-comparative time series analysis to a large data set of neonatal vital signs and found new time series measures that were highly effective in detecting physiological signatures of illness.
King WE, Carlo WA, O’Shea TM, Schelonka, HRC neurodevelopmental follow-up investigators. Journal of Pediatrics 2022. 242: 137-144.e4. doi: 10.1016/j.jpeds.2021.11.026. PMID: 34798080
We hypothesized that a cumulative heart rate characteristics (HRC) index in real-time throughout the neonatal intensive care unit (NICU) hospitalization, alone or combined with birth demographics and clinical characteristics, can predict a composite outcome of death or neurodevelopmental impairment (NDI).
Monfredi OJ, Keim-Malpass J, Moorman JR. Physiological Measurement 2021. Doi: 10.1088/1361-6579/ac2130. PMID: 34580243
We give clinical and physiological justification for the primary importance of continuous cardiorespiratory monitoring in predictive analytics monitoring.
Moorman JR. LP. Appl Clin Inform 2021 Aug;12(4):888-896. doi: 10.1055/s-0041-1735183. Epub 2021 Sep 22.
We describe the lessons learned from experience implementing predictive analytics monitoring at an academic center and a community hospital: explain the science, don’t impact workflow, engage all levels, tailor the education, integrate into care, and follow up with support.
Callcut RA, Xu Y, Moorman JR, Tsai C, Villaroman A, Robles AJ, Lake DE, Hu X, Clark MT. Physiological Measurement 2021 PMID: 34580242 doi: 10.1088/1361-6579/ac2264
At the University of California – San Francisco, we externally validated algorithms for early detection of respiratory failure leading to urgent unplanned intubation that were developed in Medical and Surgical ICUs at the University of Virginia.
Horton WB, Barros A, Clark MT, Moorman JR. 2021. Crit Care Med. 2022 Mar 1;50(3):e221-e230. doi: 10.1097/CCM.0000000000005171
We developed predictive models for severe hypoglycemia leading to urgent therapy in ICU patients at the University of Virginia and externally validated the models in the MIMIC-III database. The illness signature that was present in the continuous cardiorespiratory monitoring, labs, and vital signs was similar for all ICUs but different from the signatures of sepsis, respiratory failure leading to urgent unplanned intubation, and hemorrhage leading to large unplanned transfusion.
Sepsis and Mortality Prediction in Very Low Birth Weight Infants: Analysis of HeRO and nSOFA.
Zeigler AC, Ainsworth JE, Fairchild KD, Wynn JL, Sullivan BA. Am J Perinatology 2021. doi: 10.1055/s-0041-1728829. PMID: 33971672
We analyzed the HRC index and nSOFA near blood cultures in VLBW infants relative to diagnosis and sepsis-associated mortality in a retrospective, single-center study of VLBW infants from 2011 to 2019.
Sullivan BA, Nagraj VP, Berry KL, Fleiss N, Rambhia A, Kumar R, Wallman-Stokes A, Vesoulis ZA, Sahni R, Ratcliffe S, Lake DE, Moorman JR, Fairchild KD. J Neonatal Perinatal Med. 2021;14(4):553-561. doi: 10.3233/NPM-200578. PMID: 33523025
We compared heart rate (HR) and oxygenation (SpO2) patterns as well as baseline variables and clinical signs prompting sepsis work-ups ultimately determined to be late-onset sepsis (LOS) and sepsis ruled out (SRO) at three NICUs.
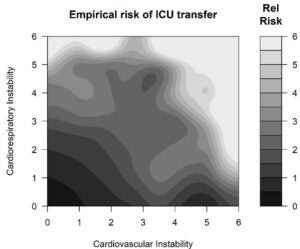
Dynamic data in the ED predict requirement for ICU transfer following acute care admission.
Glass GF, Hartka TR, Keim-Malpass J, Enfield K, Clark MT. Journal of Clinical 2021 May;35(3):515-523. doi: 10.1007/s10877-020-00500-3. Epub 2020 Mar 19. PMID: 32193694 PMCID: PMC7223530
We developed a predictive analytic tool to conduct a single-center retrospective cohort study to identify emergency department (ED) patients who required an upgrade to an intensive or intermediate care unit (ICU or IMU) within 24 hours after being admitted to an acute floor.
Davis JP, Wessels DA, Moorman JR. Crit Care Explor. 2020 Dec; 2(12): e0294. Published online 2020 Dec 18. Doi: 10.1097/CCE.0000000000000294
We review ICU scoring systems beginning with APACHE and note the evolution of the use of continuous cardiorespiratory monitoring for risk estimation in real time for subacute potentially catastrophic illnesses.
Zimmet AN, Clark MT, Gadrey S, Bell TD, Moorman JR, Moore CC. Crit Care Explor 2020 Sep 23;2(10):e0191. doi: 10.1097/CCE.0000000000000191. eCollection 2020 Oct.
We developed predictive statistical models for bloodstream infection using cases in ICU patients and blood cultures at the University of Virginia. The signature of illness reflects systemic inflammation, especially for gram-negative infections.
The relationship between acuity of organ failure and predictive validity of Sepsis-3 criteria.
Gadrey SM, Clay R, Zimmet AN, Lawson A, Oliver S, Richardson E, Forrester V, Andris RT, Rhodes GT, Voss JD, Moore CC, Moorman JR. Critical Care Explorations. 2020 2:e0199. doi:10.1097/CCE.0000000000000199. PMID: 33063019
We found that the baseline, pre-sepsis SOFA points have as much or more impact on prognosis than the ones that sepsis brings.
Early detection of in-patient deterioration: one prediction model does not fit all.
Blackwell JN, Keim-Malpass J, Clark MT, Kowalski RL, Najjar SN, Bourque JM, Lake DE, Moorman JR. Critical Care Explorations. 2020; 2(5):e0116. doi: 10.1097/CCE.0000000000000116. eCollection 2020. PMID: 32671347
We reviewed the individual EHRs of patients who deteriorated and required escalation to ICU care. The clinical scenarios were varied, and models that predicted one kind of deterioration did not work well for patients who deteriorated in a different way.
Spaeder MC, Moorman JR, Tran CA, Keim-Malpass J, Zschaebitz JV, Lake DE, Clark MT. Pediatric Research.2019. PMID:31365920
In the individual review of 1425 consecutive admissions of 1171 PICU patients, we found 187 cases of sepsis in 154 patients (blood culture for suspicion of infection, 2 or more SIRS criteria in the past 12 hours, antibiotics for more than 6 hours, and no sepsis diagnosis in past 14 days. Multivariable models had an ROC area of 0.75, and random forest captured the details of the association of age with risk better than logistic regression.
Keim-Malpass J, Clark MT, Lake DE, Moorman JR. Journal of Clinical Monitoring and Computing. 2019. PMID 31327101
We reviewed the individual EHRs of patients on a cardiology and cardiac surgery floor whose predictive analytics monitoring scores spiked from a low baseline to a high-risk level. We found that the positive predictive value of such a spike was 25% for an acute adverse event.
Pre-Vent: the prematurity-related ventilatory control study.
Dennery PA, Di Fiore JM, Ambalavanan N, Bancalari E, Carroll JL, Claure N, Hamvas A, Hibbs AM, Indic P, Kemp J, Krahn KN, Lake D, Laposky A, Martin RJ, Natarajan A, Rand C, Schau M, Weese-Mayer DE, Zimmet AM, Moorman JR. Pediatr Res. 2019 May;85(6):769-776. doi: 10.1038/s41390-019-0317-8. Epub 2019 Feb 1. PMID: 31365920
We review the Prematurity-Related Ventilatory Control Study which aims to analyze the under-utilized cardiorespiratory continuous waveform monitoring data to delineate mechanisms of immature ventilatory control in preterm infants and identify predictive markers.
Kitzmiller RR, Vaughan A, Skeeles-Worley A, Keim-Malpass J, Yap TL, Lindberg C, Kennerly S, Mitchell C, Tai R, Sullivan BA, Anderson R, Moorman JR. Applied Clinical Informatics. 2019 (2):295-306. PMID: 31042807
We describe neonatal intensive care unit clinician perceptions of a continuous predictive analytics technology and how those perceptions influenced clinician adoption.
Ruminski CM, Clark MT, Lake DE, Kitzmiller RR, Keim-Malpass J, Robertson MP, Simons TR, Moorman JR, Calland JF. Journal of Clinical Monitoring and Computing. 2018. PMID:30121744
We reviewed the individual EHRs of more than 4000 patients admitted to a surgical and a medical ICU in the 6 months before and after the deployment of the CoMET monitor in the surgical ICU. The major finding is that the rate of septic shock fell by 50% in the surgical ICU, where the display was shown, but by 10% in the medical ICU, where it was not shown. The fall was statistically significant after taking age and illness severity into account.
Dynamic data monitoring improves predictive analytics for failed extubation in the ICU.
Keim-Malpass J, Enfield KB, Calland JF, Lake DE, Clark MT. Physiol Meas. 2018 Jul 16;39(7):075005. doi: 10.1088/1361-6579/aace95. PMID: 29932430
We hypothesized that dynamic monitoring of cardiorespiratory data, vital signs, and lab test results would add information to standard clinical risk factors through conducting a retrospective observational cohort admitted to either the medical or surgical/trauma ICU that was intubated during their ICU stay and had available physiologic monitoring data.
Keim-Malpass J, Kitzmiller RR, Skeeles-Worley A, Lindberg C, Clark MT, Tai R, Calland JF, Sullivan K, Moorman JR, Anderson RA. Critical Care Nursing Clinics of North America. 2018; 30:273-87. PMID:29724445
We review the processes needed to evoke clinical action after initiation of continuous predictive analytics monitoring in an LHS.
Blackburn HN, Clark MT, Moorman JR, Lake DE, Calland JF. Surgery. 2018;163:811-818. PMID:29433853
We examine the other side of the coin – if rising risk means an imminent adverse event, does a low risk mean a good outcome?
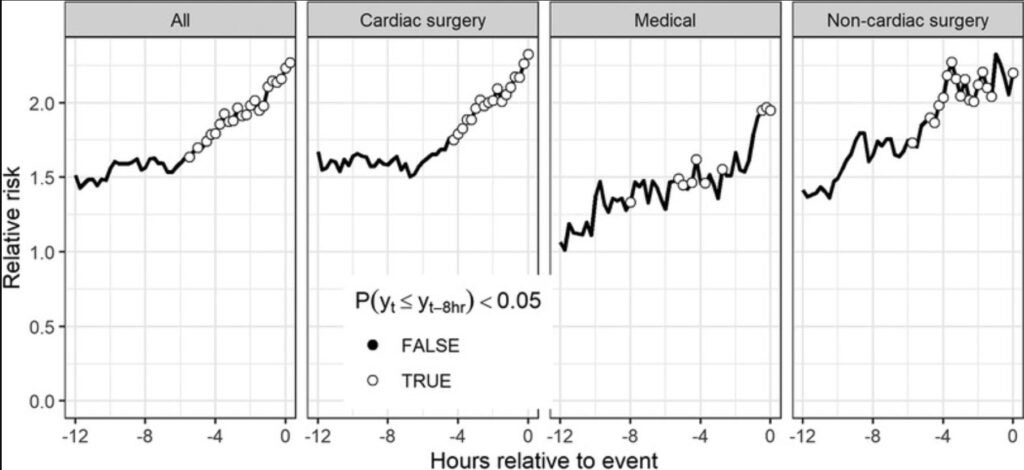
Moss TJ, Clark MT, Calland JF, Enfield KB, Voss JD, Lake DE, Moorman JR. PLoS ONE.2017;12(8):e0181448. doi: 10.1371/journal.pone.0181448. eCollection 2017.PMID: 28771487
In more than 8000 patients in an EKG-monitored cardiology and cardiac surgery ward, we tested the hypothesis that there were signatures of illness in the 700 who were transferred emergently to ICUs. The major result was that each stream of data we tested– cardiorespiratory dynamics from the EKG, lab test results, and nurse-charted vital signs – contributed to detecting deterioration and that the most effective models used all three inputs. The hypotheses were also tested using multivariable statistical models – these are the basis of some of our ward predictive analytics monitoring models.
New-onset atrial fibrillation in the critically ill.
Moss TJ, Calland JF, Enfield KB, Gomez-Manjarres DC, Ruminski C, DiMarco JP, Lake DE, Moorman JR. Critical Care Medicine. 2017.
We applied our atrial fibrillation detection algorithm to EKG monitoring of more than 8356 ICU patients and found 19% had new-onset atrial fibrillation, nearly half of which was not recognized.
Blackburn HN, Clark MT, Moss TJ, Young JS, Moorman JR, Lake DE, Calland JF. Surgery. 2017. 161(3):760-770. PMID:27894709
We aimed to externally validate a previously developed, vital sign-based, intensive care unit respiratory instability model on a separate population of intermediate care patients to test whether early detection should result in decreased mortality, duration of stay, and/or resource use.
De Pasquale M, Moss T, Cerutti S, Calland J, Lake D, Moorman JR, Ferrario M. IEEE J Biomed Health Inform. 2017:PMID:2842269
We established an early detection model for hemorrhage by exploring the range of data mining methods currently available. We then compared prediction models utilizing continuously measured physiological data from bedside monitors to those using commonly obtained laboratory tests by studying patients admitted to the University of Virginia Health System Surgical Trauma Burn ICU.
Acute noncardiovascular illness in the Cardiac Intensive Care Unit.
Holland EM, Moss TJ. Journal of the American College of Cardiology.
2017;69:1999-2007. PMID: 28427574
We performed multivariate statistical analyses to determine the association of acute noncardiovascular illnesses with outcomes, including length of stay (LOS), mortality, and hospital readmission by studying admissions to the CICU at the University of Virginia Health System between October 2012 and November 2014.
Computers in white coats: how to devise useful clinical decision support software.
Moorman JR, Lake DE, Moss TJ. Critical Care Medicine. 2016;44(7):1449-1450.
This editorial outlines our approach to predictive analytics monitoring modeling and implementation: pick the right problem, look at the data, fear no math, and do clinical trials.
Moss TJ, Lake DE, Calland JF, Enfield KB, Delos JB, Fairchild KD, Moorman JR. Critical Care Medicine.2016;44(9):1639-1648 doi: 10.1097/CCM.0000000000001738. PMID: 27452809 PMC4987175.
In more than 9000 patients (8636 adults, 601 premature neonates) our ICUs, we tested the hypothesis that there were detectable physiological signatures of illness in the continuous monitoring data. The main results were that respiratory failure and hemorrhage presented with similar cardiorespiratory dynamics in the adult medical and surgical ICUs: sepsis, however, presented differently in medical vs surgical patients. In infants, on the other hand, there was only one signature of illness. The hypotheses were tested using multivariable statistical models – these are the basis of some of ICU predictive analytics monitoring models.
Heart rate dynamics preceding hemorrhage in the intensive care unit.
Moss TJ, Clark MT, Lake DE, Moorman JR, Calland JF. J Electrocardiology. 2015;48:1075-80
We studied consecutive admissions to the STICU at the University of Virginia Health System, collected ECG waveform data, and calculated linear and non-linear measures of the RR interbeat intervals to test the hypothesis that a transfusion requirement of 3 or more PRBC transfusions in 24 hours is preceded by dynamical changes in heart rate measures and performed logistic regression modeling.
Predicting the need for urgent intubation in a surgical/trauma intensive care unit.
Politano AD, Riccio LM, Lake DE, Rusin CG, Guin LE, Josef CS, Clark MT, Sawyer RG, Moorman JR, Calland JF. Surgery. 2013 Nov;154(5):1110-6. doi: 10.1016/j.surg.2013.05.025. Epub 2013 Sep 26. PMID: 24075272
We analyzed and modeled data monitoring vital signs and waveforms in patients in a surgical/trauma intensive care unit (STICU), which could allow for early identification and treatment of patients with evolving respiratory failure by collecting vital sign and waveform data for STICU patients between February 2011 and March 2012.
Septicemia mortality reduction in a heart rate characteristics monitoring trial.
Fairchild KD, Schelonka RL, Kaufman DA, Carlo WA, Kattwinkel J, Porcelli PJ, Navarrete CT, Bancalari E, Aschner JL, Walker MW, Perez JA, Palmer C, Lake DE, O’Shea TM, Moorman JR. Pediatric Research 2013. 74: 570-5. PMID: 2394255
We hypothesize that the reduction in mortality is due to a decrease in septicemia-associated mortality.
Moorman JR, Carlo WA, Kattwinkel J, Schelonka RL, Porcelli PJ, Navarrete CT, Bancalari E, Aschner JL, Whit Walker M, Perez JA, Palmer C, Stukenborg GJ, Lake DE, Michael O’Shea T. Journal of Pediatrics. 2011;159(6):900- 6.e1 PMC3215822.
This is the largest individually randomized clinical trial in the field of neonatology, and showed a survival benefit in premature infants whose risk of imminent sepsis was displayed to clinicians. It establishes the principle that predictive analytics monitoring saves lives.
Physiological time-series analysis using approximate entropy and sample entropy.
Richman JS, Moorman JR.
Am J Physiol Heart Circ Physiol. 2000 Jun;278(6):H2039-49. Doi: 10.1152/ajpheart.2000.278.6.H2039. PMID: 10843903
We describe a new approach to the estimation of Kolmogorov-Sinai entropy in short, noisy time series. The new measure, sample entropy, has gone on to a life of its own in the field of non-linear dynamical analysis (cited >5000 times in ISI and >7000 times in Google Scholar). Fundamentally, the measure is the negative logarithm of the probability that two segments of length m in a time series, having matched within a tolerance r, will also match at the next, or m+1st point.
Sample entropy analysis of neonatal heart rate variability.
Lake DE, Richman JS, Griffin MP, Moorman JR.
Am J Physiol Regul Integr Comp Physiol. 2002 Sep;283(3):R789-97. doi: 10.1152/ajpregu.00069.2002. PMID: 12185014
We describe the mechanism by which the sample entropy measure detects heart rate time series with reduced variability and transient decelerations, the abnormal heart rate characteristics of neonatal sepsis. We also address fundamental numerical problems in entropy estimation, especially that of picking the tolerance r for allowing points to match.
Lake DE, Moorman JR.
Am J Physiol Heart Circ Physiol. 2011 Jan;300(1):H319-25. doi: 10.1152/ajpheart.00561.2010. Epub 2010 Oct 29. PMID: 21037227
We describe an optimal estimation of sample entropy of heart rate and employ quadratic entropy rate to remove the problem of picking the tolerance r for matches. We call the new measure the coefficient of sample entropy and describe its performance in detecting atrial fibrillation.
DeMazumder D, Lake DE, Cheng A, Moss TJ, Guallar E, Weiss RG, Jones SR, Tomaselli GF, Moorman JR.
Circulation (Arrhythmia and Electrophysiology). 2013;6(3):555-561.
We hypothesize that the higher entropy of rapid cardiac rhythms preceding ICD shocks distinguishes AF from VT/ventricular fibrillation by conducting a multicenter, prospective, observational study of patients with primary prevention ICDs where patients received shocks from ICDs with stored, retrievable intracardiac electrograms.
Local dynamics of heart rate: detection and prognostic implications.
Moss TJ, Lake DE, Moorman JR.
Physiol Meas. 2014 Oct;35(10):1929-42. doi: 10.1088/0967-3334/35/10/1929. Epub 2014 Sep 17.
We devise a new non-linear measure of heart rate dynamics based on as few as 12 beats that distinguishes heart failure patients from normal controls and has strong prognostic implications.
Carrara M, Carozzi L, Moss TJ, de Pasquale M, Cerutti S, Ferrario M, Lake DE, Moorman JR. Physiol Meas. 2015 Sep;36(9):1873-88. doi: 10.1088/0967-3334/36/9/1873. Epub 2015 Aug 6. PMID: 26246162
We develop multivariable statistical models using logistic regression and random forests for categorizing short heart rate time series and find a superior performance of non-linear metrics, including coefficient of sample entropy and local dynamics score. The resulting algorithms have good performance in distinguishing atrial fibrillation not only from normal sinus rhythm but also from sinus rhythm with as little as 10% ectopic burden.
Lensen IS, Monfredi OJ, Andris RT, Lake DE, Moorman JR.
JRSM Cardiovasc Dis. 2020 Aug 26:9:2048004020948732. doi: 10.1177/2048004020948732. eCollection 2020 Jan-Dec. PMID: 32922768
We demonstrate how heart rate fragmentation gives novel insights into non-autonomic mechanisms of beat-to-beat variability in cycle length, and predicts survival of cardiology clinic patients, over and above traditional clinical risk factors and measures of heart rate variability by studying patients seen by cardiologists with clinical data including 24-hour Holter monitoring.
Imputation of partial pressures of arterial oxygen using oximetry and its impact on sepsis diagnosis. Gadrey SM, Lau CE, Clay R, Rhodes GT, Lake DE, Moore CC, Voss JD, Moorman JR.
Physiological Measurement 2019 Dec 3;40(11):115008. doi: 10.1088/1361- 6579/ab5154.
We relate the oxygen saturation to the SOFA respiratory component score using a new model-based equation.