Larry Borish, MD

PRIMARY APPOINTMENT:
Professor of Medicine and Microbiology
CONTACT:
PO Box 801355
Telephone: 434-243-2610
Email: lb4m@virginia.edu
EDUCATION AND TRAINING:
- MD, Boston University School of Medicine, Boston, MA
- Residency, Internal Medicine, Harvard Medical School – New England Deaconess Hospital, Boston, MA
- Fellowship, Tufts Medical School – New England Medical Center, Boston, MA
FUNDED PROJECTS:
- Clinical response to rhinovirus challenge in human asthmatics (NIAID)
- : Lung rhinovirus (RV) infection identifies pre-school children with type 2 inflammation at risk for the development of asthma (NIAID)
- IgE-independent mast cell activation by food-derived peptides in eosinophilic esophagitis (NIAID)
- NHLBI PrecISE Interventions for Severe and/or Exacerbation Prone Asthma (NHLBI)
- Systemic Allergic Reactions to SARS-CoV2 Vaccination (NIAID)
- A Phase 3, Randomized, 3-Part Study to Investigate the Efficacy and Safety of Dupilumab in Adult and Adolescent Patients with Eosinophilic Esophagitis (Regeneron Pharmaceuticals, Inc.)
- Interleukin-5 receptor in COPD (GlaxoSmithKline, LLC)
- Undetectable IgE as a sentinel biomarker for humoral immunodeficiency (CSL Behring, LLC)
- Viral infection in asthma (VIA) study (Regeneron Pharmaceuticals, Inc.)
RESEARCH AREAS:
- Innate immune mechanisms of rhinovirus (RV)-induced asthma exacerbations. Immune and cellular mechanisms of asthma. Immune mechanisms in chronic hyperplastic eosinophilic sinusitis (CHES).
RESEARCH SUMMARY:
Current research focuses on the innate immunity-mediated mechanisms by which rhinovirus (RV) exacerbates asthma. The greatest morbidity associated with asthma is the occurrence of severe, potentially life-threatening exacerbations. RV accounts for ~60-70% of childhood and adolescent asthma exacerbations. Although an exacerbation would be predicted whenever a cytopathic inflammatory response is superimposed upon the asthmatic lung, this is not what is observed – and only RV infections are consistently associated with asthma exacerbations. RV-associated asthma exacerbations are linked to the presence of an increased type 2 cytokine signature (IL-4, IL-5, and IL-13). My laboratory’s studies investigate innate immune mechanisms underlying a type 2 immune deviating signature. In particular, we are interested in the roles of epithelial-derived IL-25/IL-33/TSLP and the specific cell source of these cytokines including specialized cells such as neuroendocrine and solitary chemosensory cells. We have confirmed the dogma that the asthmatic airway displays evidence for reduced interferon-mediated antiviral immunity but find no evidence for this having an impact on viral clearance, indeed, asthmatics display lower viral loads. These investigations argue that the enhanced compensatory mechanism of type 2 (eosinophilic) inflammation is responsible for driving viral clearance. However, this alternative, eosinophil-mediated anti-viral responses evolves only at the cost of worsening asthmatic symptoms.
In addition to these UO1-funded studies, my RV-asthma research is further supported by an R21 that investigates evidence for nascent type 2 inflammation in the lungs of pre-school children with problematic wheeze undergoing clinically indicated bronchoscopies in whom rhinovirus (RV) infection is identified. In addition, for the next 2½ years, the Borish laboratory will be the co-lead sponsor of a Regeneron-funded investigator-initiated study entitled “Viral infection in asthma (VIA) Study: A randomized, placebo-controlled study to assess cellular and molecular markers related to experimental rhinovirus infection in mild asthmatics, and the effect of dupilumab in this investigational model.” The goal of this study will be to assess the molecular and cellular basis by which dupilumab prevents the development of an RV-induced asthma exacerbation.
Unrelated to the RV studies, the Borish lab continues to collaborate closely with Dr. Gerry Teague in pediatrics as co-PI for the UVA commitment to the NHLBI-funded PreCISE Asthma Network Clinical Centers. These are studies that will enroll severe treatment-resistant asthmatics and investigate novel therapeutics in this refractory population.
Finally, we also have several investigator-initiated pharmaceutical studies. Currently, we are enrolling patients in a GSK sponsored study to investigate type 2 inflammation in COPD and more specifically the expression of IL-5 receptor on airway neutrophils. And, lastly, we are supported by a Regeneron-funded investigator-initiated award involving the role of dupilumab in attenuated staphylococcus aureus infection in chronic sinusitis and amelioration of the dysbiotic state.
Research Team
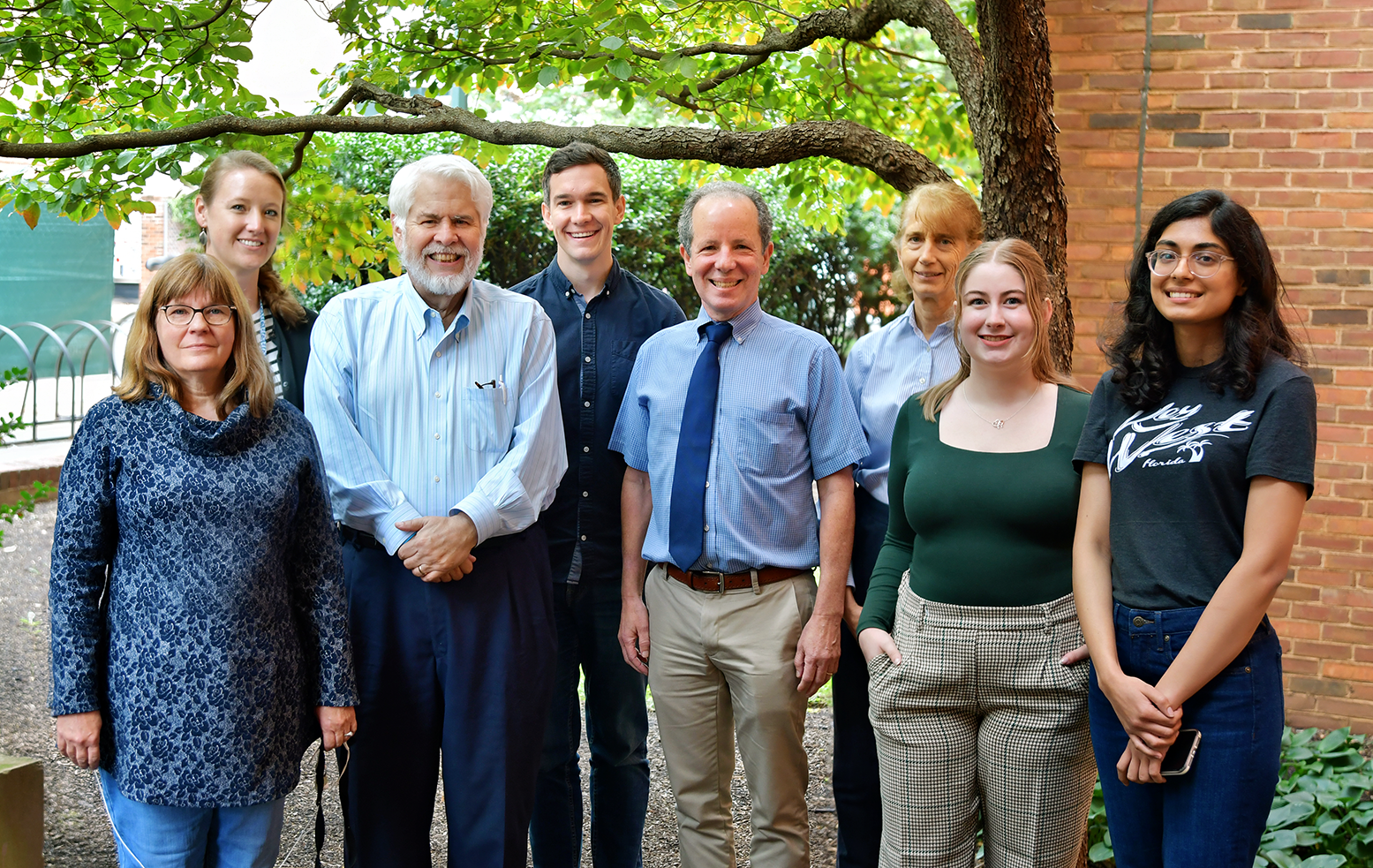
From left, first row: MarthaJoy Spano, W. Gerald Teague, Larry Borish, Rebecca Revell, Khyati Menghani Back row: Kristin Wavell, Cameron Griffiths, and Elaine Etter
 Senior Scientist
Senior Scientist
(Bio coming soon)

 Clinical Research Coordinator
Clinical Research Coordinator
Khyati joined the division in 2023, and her research interests primarily focus on the role of biologics in moderate to severe asthmatics. Under the guidance of Dr. Nelson, she has gained valuable insights into the field. She completed her MBBS degree in India and plans to pursue a medical residency in the near future.
Outside of work, she enjoys swimming and practicing yoga.
 Clinical Research Coordinator
Clinical Research Coordinator
Rebecca earned her B.S. in Public Health from Virginia Tech / VMCVM
Research Interests include the Epidemiology of eosinophilic esophagitis (EoE), improving diagnostic testing in eosinophilic esophagitis (EoE), and improving patient experience and continuity of care during pediatric to adult care transition. Rebecca loves cooking, baking, and hosting get-togethers, especially around the holidays. She is originally from Massachusetts, where her family has lived in the same house since ~1750.

Lab Manager
MarthaJoy grew up in the Chicago area and attended college and graduate school in the Boston area. She received a BA in Biochemistry and a Masters in Biochemistry. She has worked in industry (pharmaceutical, chromatography, and antibody use and development) and academia (crystallography, cell biology, immunology, allergy/immunology). To quote MarthaJoy: “While research science may not have been the stable field for employment that I thought it was, it is always the most interesting”.
RN Care Coordinator
Deb earned her nursing degree from the University of Virginia and has been at UVA for over 46 years. She works closely with the Borish lab, studying the innate immunity-mediated mechanisms by which rhinovirus (RV) exacerbates asthma. In her spare time, Deb enjoys biking, baking, and taking care of her three dogs, Binx, Ryder, and Zane.
Selected Publications
-
- Kennedy, J.L., M. Shaker, V. McMeen, J. Gern, H. Carper, D. Murphy, W-M Lee, YA Bochkov, R.F. Vrtis, T. Platts-Mills, J. Patrie, L. Borish, J.W. Steinke, W.A. Woods, and P. Heymann. 2014. Comparison of viral load in individuals with and without asthma during infections with rhinovirus. J. Respir Crit Care Med. 189(5):532-9.
- Steinke, J.W., L. Liu, R.B. Turner, T.J. Braciale, and L. Borish. 2015. Immune surveillance by rhinovirus-specific circulating CD4+ and CD8+ T lymphocytes. PlosOne DOI:10.1371/ journal.pone.0115271 January 13, 2015.
- Hamed A, Preston DC, Eschenbacher W, Khokhar D, Workam L, Steinke JW, Heymann P, Lawrence M, Soto-Quiros M, Platts-Mills TAE, Payne S, Borish L. 2019. Nasal IgE production in allergic rhinitis: Impact of rhinovirus infection. Clin Exp Allergy. Jun;49(6):847-852
- Heymann P, TAE Platts-Mills, JA Woodfolk, L Borish, D Murphy, HT Carper, M Conaway, J Patrie, JW Steinke, L Muehling, WG Teague, JL Kennedy, A-M Irani, M McGraw, S Early, RB Turner. Understanding the asthmatic response to an experimental infection with rhinovirus: Using the administration of omalizumab to explore the effects of blocking IgE. J Allergy Clin Immunol. 2020 Feb 1. pii: S0091-6749(20)30124-X. doi: 10.1016/j.jaci.2020.01.035.
