Rahul Sharma, PhD Lab
PRIMARY APPOINTMENT
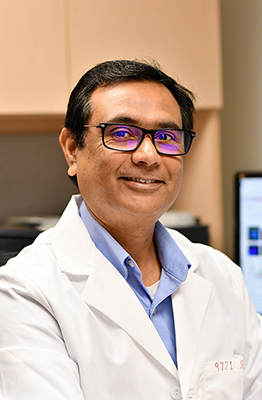
Associate Professor, Medicine: Nephrology
Contact:
UVA Division of Nephrology
Center for Immunity Inflammation and Regenerative Medicine, Division of Nephrology, PO Box 800133
Charlottesville, VA 22908
phone: 434-247-7753
Email: rs3wn@virginia.edu
EDUCATION AND TRAINING
- MSc, Animal Biochemistry, National Dairy Research Institute
- PhD, Genetic Engineering, University of Delhi
RESEARCH AREAS
Regulatory T Cell biology in Inflammatory and Autoimmune Diseases.
CURRENT LABORATORY MEMBERS
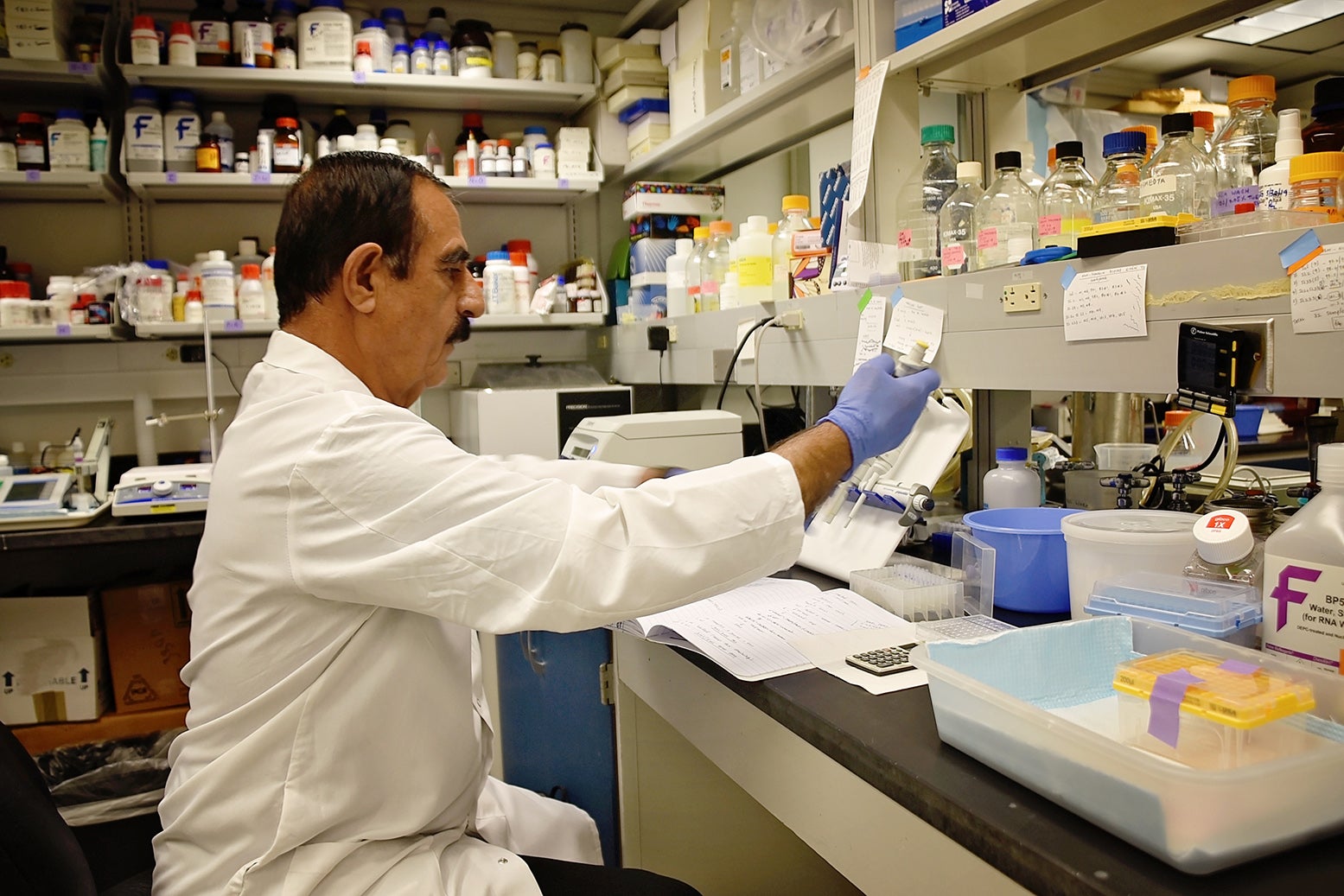
Saleh Mohammad, BS (Nursing)
Laboratory Technician
Contact:
Originally from Afghanistan, Saleh has worked and lived in many Asian and European countries as a trained nurse. Saleh has been working with Dr. Sharma since 2013 and has played a central role in managing mouse colonies and laboratory upkeep. He has been collecting data on the function of salivary glands, kidneys, and pancreas in animal models. He is one of the most skilled persons in cryo-sectioning and mouse phlebotomy. Saleh’s hobbies include making friends, helping others, and watching movies.
Fun fact: Saleh shares his lunch with someone every day. You will undoubtedly feel lucky if you have tried his delicious “Kismet rice.”
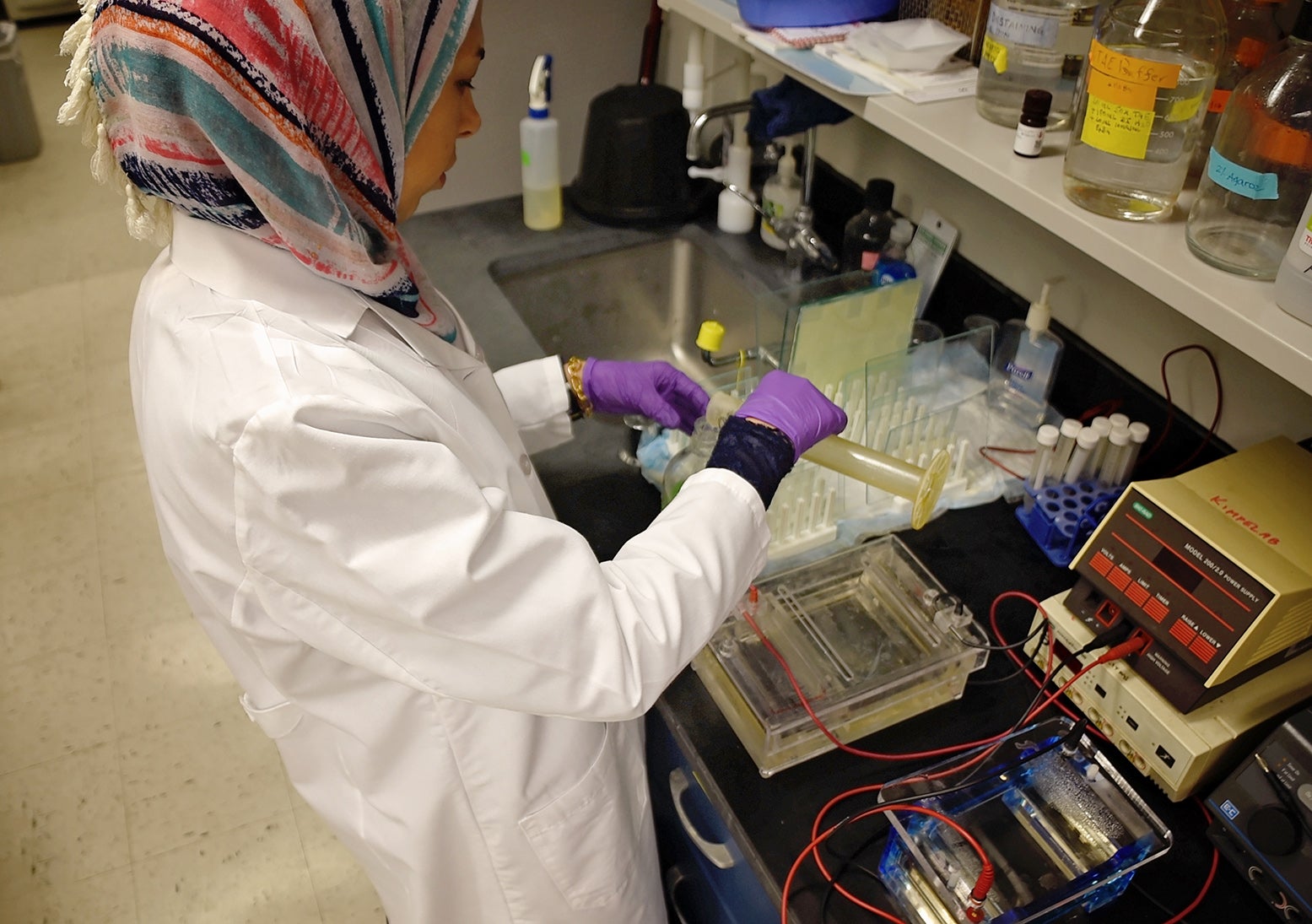
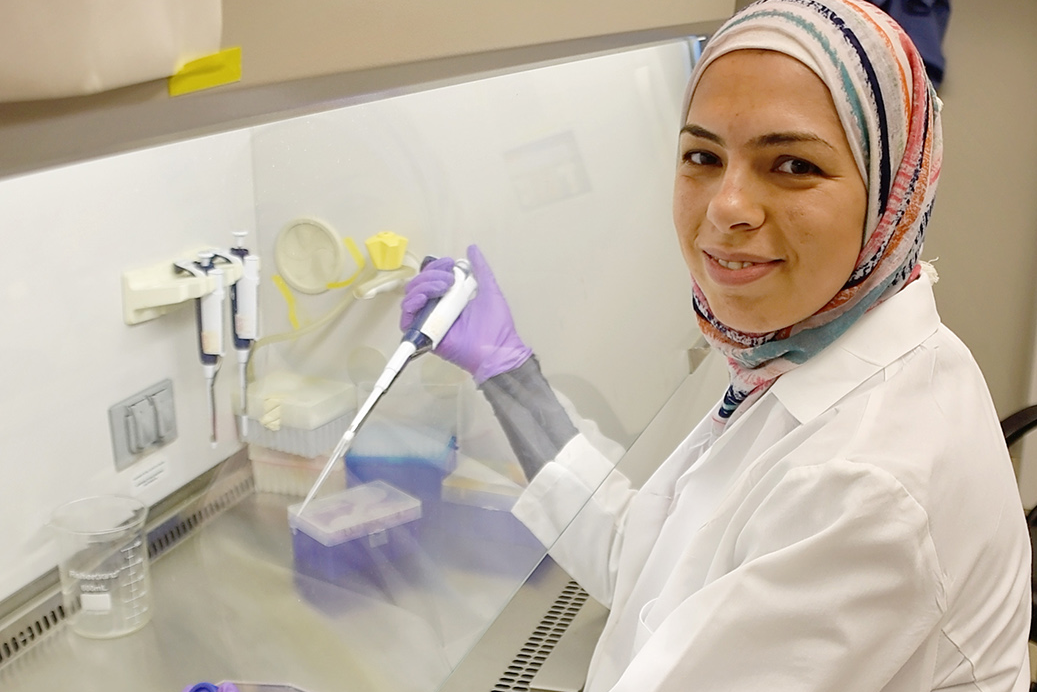
Hiba Mohammed, BS
Laboratory Assistant
Contact:
Hiba originally hails from Iraq and has been working on the human AKI and PD1 projects. She is helping all the lab members with mouse processing of clinical samples and mouse genotyping. She is an enjoyable person and is busy raising her three children along with her husband when not working in the lab.

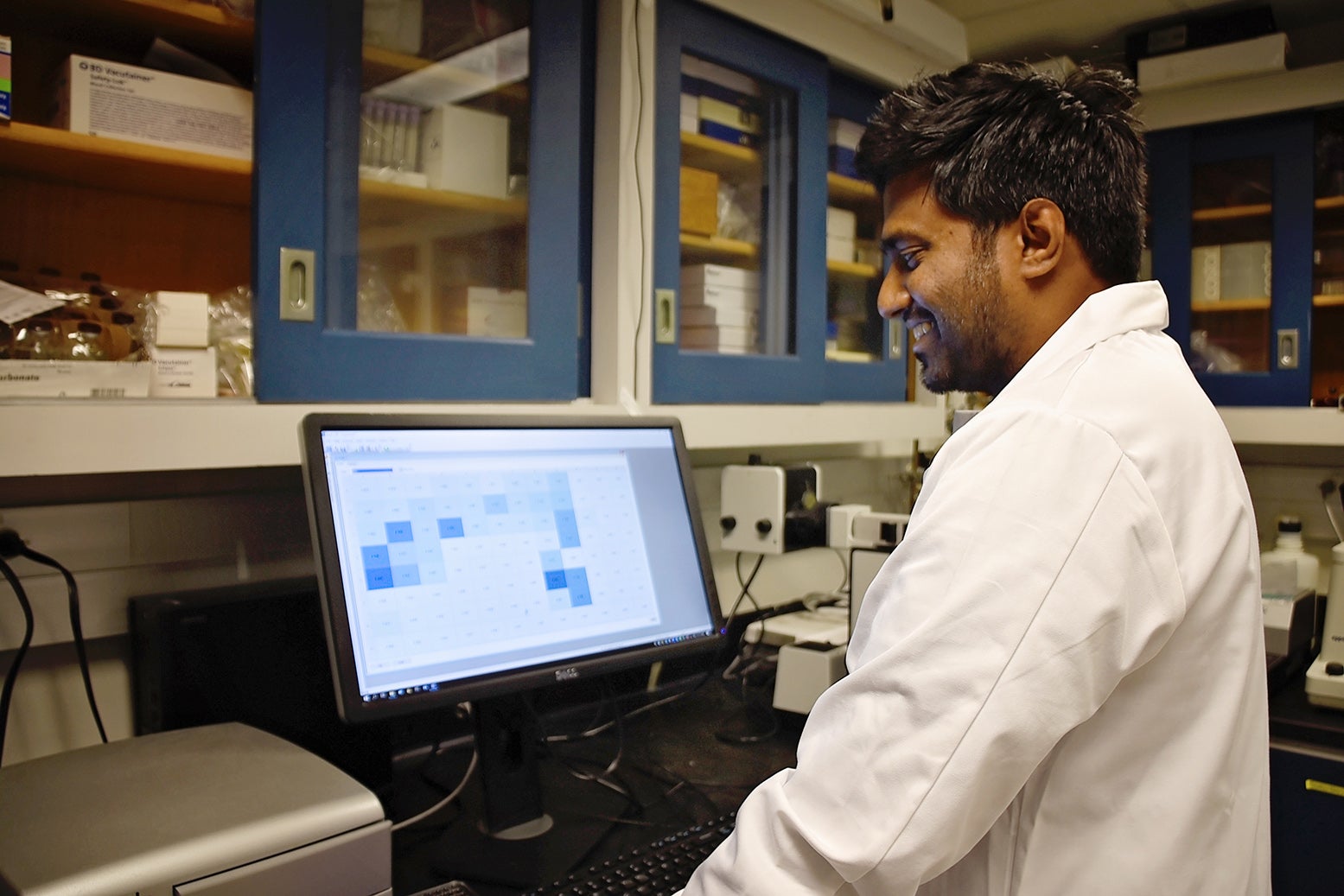
Vikram Sabapathy, PhD
Research Associate
Contact:
Vikram received his PhD. from the Centre for Stem Cell Research, Christian Medical College, Vellore. His PhD. thesis with Dr. Sanjay Kumar broadly deals with the characterization of perinatal Mesenchyman Stem Cells (MSC), the generation of safer human induced Pluripotent Stem Cells (iPSCs), and tissue engineering studies for translational applications. In particular, he is interested in understanding the complex aspects of cellular reprogramming, tissue repair, and regeneration.
He joined the laboratory of Dr. Rahul Sharma as a Research Associate at the Center of Immunity, Inflammation, and Regenerative Medicine (CIIR), University of Virginia, to understand the immune system’s role in regenerative medicine. The immune system poses a great challenge for the translational application.
Presently, he is exploring the importance of T regulatory cells (Tregs) / innate lymphoid cells (ILC2s) using rodent kidney injury and diabetes models. Additionally, Vikram is also involved in characterizing progenitor cells in the kidney and the development of organoids for disease modeling and drug discovery applications.
In his spare time, he unwinds by listening to music, exercising, and reading short stories.

Airi Price
UVA Class of 2021
Contact:
Airi is a third-year undergraduate at UVA studying Medical Anthropology and Environmental Sciences. In the lab, she studies the interaction of immune cells with renal and islet progenitor cells. The NIH STEP-UP and UVA Harrison Undergraduate Research Awards support her participation in the Sharma lab. She also manages the stock of laboratory mice with Dr. Vikram Sabapathy to assist in various projects.
Airi enjoys traveling, swimming, and long walks with her dog in her free time. She recently completed a clinical project in Rwanda, Africa, to understand the issues in the medical care of underprivileged patients.
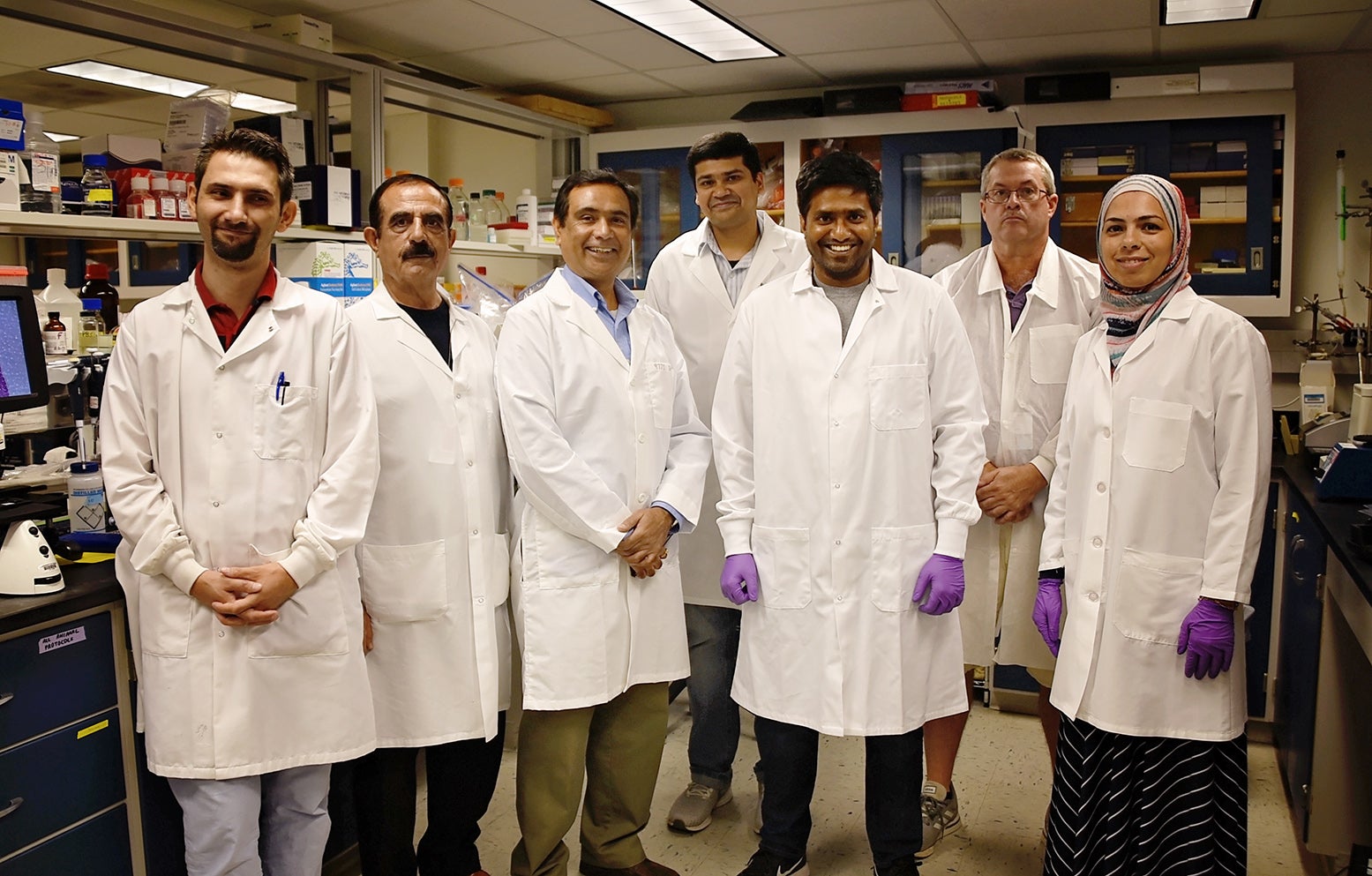
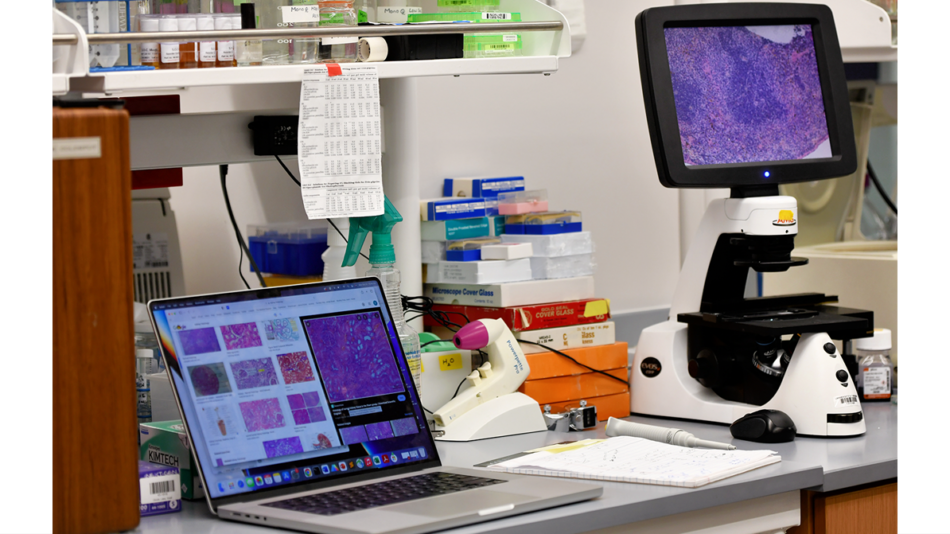
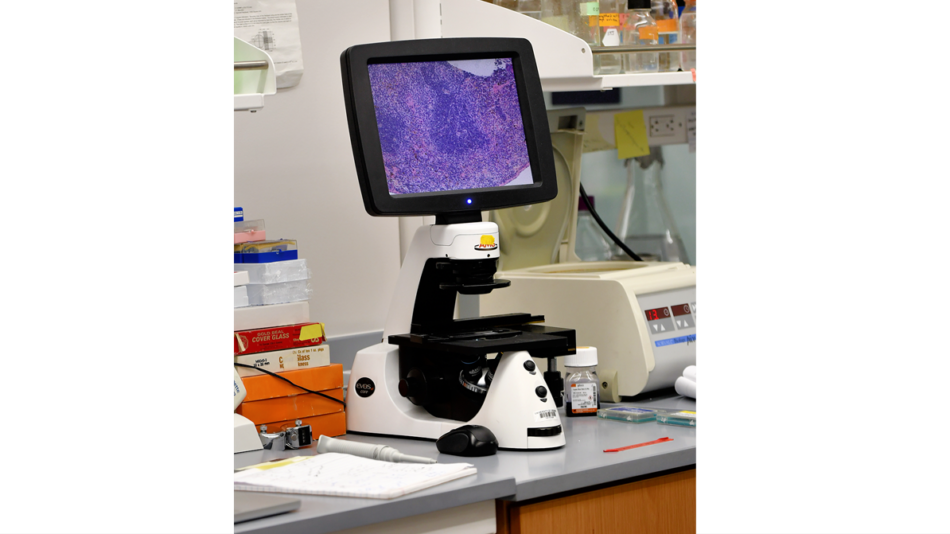
Lab Team Images
RESEARCH SUMMARY
The long-term goal of our research is to identify and produce novel therapeutic agents which have the potential to translate from bench to bedside. Our major interest lies in autoimmune and inflammatory diseases with a focus on the Regulatory T-cells, a specialized helper-T cell subset that prevents abnormal immune system activation. We are exploring the role of alarmins and stress-related molecules in the biology of regulatory T-cells. The broad hypothesis is that acute stress signals, which induce recruitment of inflammatory cells for clearance of danger and pathogenic signals can be exploited to promote regulatory T cells for therapy of inflammatory disorders. Autoimmunity is regulated by two major factors (1) genetic predisposition and (2) environmental insult. Since genetics cannot be altered, we are invested in identifying the environmental/microenvironmental insults that may trigger an autoimmune reaction. The disease models we study are related to the pancreas and kidneys, such as type 1 and type 2 diabetes, diabetic kidney diseases, acute kidney injury (which affects up to 30% of all ICU patients), and lupus nephritis. Collectively these diseases are now the largest cause of human morbidity and mortality.
Active Projects
-
- Modulating homeostasis of immune-regulatory lymphocytes: Regulatory T cells (Treg) exert the major mechanism of peripheral tolerance. Treg deficiency causes early mortality in mice and humans due to multi-organ autoimmune syndrome. Most, if not all, autoimmune disorders are now being attributed to either numerical deficiency or functional inefficiency of the Tregs. We study the interplay of Treg and auto-reactive T cells, in terms of their homeostasis, effector function, and migration/homing to the sites of inflammation. We have shown that IL-2 signaling plays an essential role in these processes. Our studies use various mutant and knockout mice predisposed to autoimmune defects. We have developed several rapid and efficient models of Treg-deficiency-based abnormalities that find applications in studies on autoimmune diseases, including Allergic dermatitis, Psoriasis, Autoimmune pulmonary inflammation, Sjogrens syndrome, Type 1 diabetes, and Ulcerative colitis (Inflammatory Bowel Disease). My laboratory identifies novel druggable targets and generates therapeutic reagents to enhance regulatory T-cells homeostasis. We have identified several pathways which are regulated by IL-2 and can be targeted pharmacologically for intervention in autoimmune and inflammatory diseases. One of these targets is the alarmin IL-33. We identified that IL-2 regulates the expression IL-33 receptor on Tregs, and IL-33 can promote their function and homeostasis. We have generated a novel reagents IL233 (a hybrid of IL-2 and IL-33), which not only prevents inflammation but also can induce remission in animal models of established diseases, including Lupus Nephritis, Type I Diabetes, Type 2 Diabetic Nephropathy, Hypertension, and Acute Kidney Injury. Our studies have developed further leads for the roles of IL-2/IL-33 axis, regulatory T-cells, and innate lymphoid cells in the regeneration of injured tissue.
- PD-1 pathway and T-regulatory cells in Acute Kidney Injury: This is an NIH-funded collaborative project between the Sharma Lab, Dr. Gilbert Kinsey, and Dr. Didier Portilla. Acute kidney injury (AKI) complicates at least 5% of all hospitalizations and up to 30% of cardiac surgeries, increasing mortality and progressing to chronic renal disease in many patients. Inflammation contributes significantly to the loss of renal function and kidney cell death. We have shown that CD4+Foxp3+ regulatory T cells (Tregs) are reno-protective lymphocytes and raise the threshold of experimental AKI. We found that expression of interleukin 10 (IL-10) and the checkpoint inhibitor programmed death 1 (PD-1) on Tregs is required. Our ongoing studies focus on the interaction of PD-1 activation on the Tregs with their metabolism, cytokine response, and PD-L1-expressing kidney epithelial and vascular endothelial cells. These mechanistic studies in mice will provide a platform for future pre-clinical and clinical studies of the therapeutic utility of Tregs and Treg-associated mechanisms in AKI.
- Circulating Renal Protective Mediators in Cardiac Surgery Patients: Acute kidney injury (AKI) after cardiac surgery requiring cardiopulmonary bypass occurs in up to 1/3 of patients. The pathogenesis of AKI involves ischemia-reperfusion injury (IRI), endothelial cell dysfunction, and activation of immune cells in the cardiopulmonary bypass circuit. A deficit of Tregs predisposes mice to kidney IRI, in this NIH-funded clinical collaborative study with Drs. Rosner, Lynch, and Kinsey, have proposed to evaluate Treg number and functional markers in adult cardiac surgery patients.
- TREX1 pathway in autoimmune diseases: The Sharma lab is also involved in understanding the role of defective clearance of DNA from necrotic and apoptotic cells in the pathophysiology of autoimmune diseases. We have identified an interplay of innate and adaptive immune cells in losing tolerance to nuclear antigens. This also results in a gradual loss of regulatory T-cells and auto-immunity progression to clinical inflammatory disease. This work is being carried out in collaboration with Dr. Fred Perrino of Wake Forest University and is funded by an NIH R01 grant.