Opportunities for Giving

Every second counts in an emergency and so does your support.
Enter for “Emergency Medicine” under the Designation field.
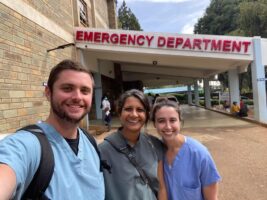
For more than 20 years, generous community donations have fueled the impactful initiatives of UVA Emergency Medicine. Your support has played a vital role in advancing medical education, fostering groundbreaking research, and enhancing technological innovation. Thanks to contributions like yours, we’ve also expanded our international partnerships, allowing us to make a difference on a global scale.
Join us in continuing this important work and help us transform lives through exceptional emergency care.
Enter for “Emergency Medicine” under the Designation field.
Give Online
Questions?
Please email our COO, Shannon Hughen-Giger, with your questions and to learn about more ways to support Emergency Medicine.
To support our ongoing mission, please use the UVA Medical Alumni Association donation link, and be sure to specify the Department of Emergency Medicine as the account destination, by choosing one of the following options:
- Emergency Medicine: Emergency Medicine Resident Education Fund
- Emergency Medicine: Department of Emergency Medicine Global Health Fund
Please make the check payable to the UVA Medical School Foundation and write the account designation on the memo line:
University of Virginia Medical School Foundation
P.O. Box 37963
Boone, Iowa 50037
Tax ID number is 23-7173411.
Other Methods: Supporting the School of Medicine (see FAQs)
Questions?
Please email our COO, Shannon Hughen-Giger, with your questions and to learn about more ways to support Emergency Medicine.
Wish List
Help us make an impact today by supporting our state-of-the-art services and scholarships.
- Rapid Pilot Micro-Grant (1 award) ~ $10,000
- Funds a 3-month pilot to collect preliminary data for an NIH/AHRQ application.
- Impact (12 months): 1–2 abstracts/manuscripts; competitive external grant submission.
- AI Research Computer (GPU Workstation) ~ $10,000
- A privacy-protecting, high-performance desktop for de-identified data analysis and rapid model prototyping.
- Impact (12 months): Cuts analysis time; enables 2–3 AI projects to reach publishable results faster.
- Wearable Health Monitoring Starter Kit ~ $9,500
- Mixed set of research-grade sensors (e.g., continuous vitals/actigraphy), chargers, and study logistics supplies for feasibility studies in the ED and hallways.
- Impact (12 months): Launches one multi-sensor pilot; generates real-world data to improve early deterioration detection.
- Resident/Student Research Scholar Stipend ~ $7,500
- Paid 6–8 week research experience (stipend + modest project costs) focused on AI, quality, or diagnostic safety.
- Impact (12 months): 1 poster at ACEP/SAEM and a co-authored manuscript; develops the next generation of clinician-scientists.
- An emergency fund, which would need to be about $20k to support 36 residents.
- Prior resident physicians have had to rely on food stamps to feed their families. They often do not have enough savings to afford emergencies such as their car breaking down or a loved one getting ill. They have to figure these things out while working over 60 hours per week in the hospital. Please consider donating to an emergency fund to support the resident physicians who work so hard to care for you and the community of Charlottesville.
- Funding for our residents studying at other institutions and providing care on humanitarian trips in rural or international areas. This would require about $15k to support 5 residents.
- Hosting 2 Kenyan students each year (includes housing, travel, visa fees, and food): $12,000
- Resident scholarships for global health rotations: $4000 per resident, 4-5 per year
- EMT and ambulance driver trainings in Nepal: $2000 per year
- Expand the testing capabilities related to novel psychoactive substances of use/misuse presenting to UVA Health’s Department of Emergency Medicine.
In order to combat the rapidly evolving plethora of drugs entering into society and specifically into Virginia, there needs to be enhanced and effective epidemiological surveillance. We are requesting funding for a 0.5 FTE laboratory technician who can dedicate time to analytical testing of samples of patients presenting to the UVA Health’s Department of Emergency following an overdose. This position would have access to UVA Health’s clinical toxicology laboratory (e.g., GC-MSMS) and would dedicate time to further expand surveillance and data dashboard pertaining to emerging novel psychoactive substances (NPS) use/misuse in our community.
The laboratory technician would work with the Department’s faculty epidemiologist to expand surveillance systems, perform statistical analysis on existing data sets, and help to provide public health improvement and education plans based on the testing results as new substances are discovered that are emerging into the community. The laboratory technician will support programs developed by the Medical Toxicology – Emergency Medicine faculty. The work will help to identify and analyze public health issues related to substance use/misuse and help to develop future scientific studies in the Department of Emergency Medicine.
Funding Request: $75,000 we cannot pay salary from donated funds
- National Student Health Auto-Uploaded Database
We are requesting funding to initiate a radical idea: develop a unified nationwide de-identified database that will track, in near real-time, student health data throughout the country that mimics the U.S. National Poison Center Database (NPDS).
In 2013, a novel idea launched at the University of Virginia by faculty in the Department of Emergency Medicine. The concept of interconnecting all student data into a single de-identified database for real-time research was submitted to UVA’s HSR-IRB. After thorough vetting and considering all applicable laws, such as HIPAA and FERPA, the project was approved and the database created (IRB-1). Student databases initially interconnected included: UVA Health’s EMR Epic including all data of students interacting with the Department of Emergency Medicine; University Student Information System (SIS); Department of Student Health & Wellness’ Electronic Medical Record (EMR) Medicat; Student Disability Access Center’s EMR AIM; Dean’s database SafeGrounds. This massive de-identified dataset, dating back to 2009, was initially launched to help determine prevalence of substance use/misuse and aid in targeting prevention efforts. This database was subsequently used for tracking and researching other injury and disease in students, such as infectious disease, concussions, and mental health. Numerous research projects launched, engaging student researchers, and the results were accepted for presentation at national meetings and publication in peer-reviewed journals. The database’s real-time capabilities were leveraged during the pandemic when daily reports were generated using the data on the true impact of COVID-19 on the student population. That real-time data enabled the university to manage outbreaks and remain open.
Interconnecting various distinct institutional datasets from across the country has occurred for years in other specialty areas. The NPDS is an example of one such system. The NPDS has been in existence for over 20 years and every 5 minutes each U.S. poison center auto-uploads de-identified data to a national repository for real-time surveillance, working in collaboration with the national organization called the American Association of Poison Control Centers (AAPCC) and governmental entities such as the CDC. Hundreds of studies have emerged from the NPDS and it has been instrumental in U.S. public health surveillance. The faculty from the Division of Medical Toxicology – Department of Emergency Medicine has worked closely with the NPDS and published research extensively from it. The idea proposed is to mimic that NPDS model and create a similar de-identified SHW national dataset that enables real-time uploading of data associated with a diverse national representative sample of higher education institutions. This national dataset has been approved by UVA (IRB-2) where such data can be uploaded. Prior to the pandemic, this concept was trialed with a sampling of major universities across the country that uploaded student specific influenza data. This enabled the tracking of influenza outbreaks across the country that included associated student demographics. In this proposal for further funding, we plan to expand markedly upon that initial trial and engage a select number of universities to copy UVA’s institutional interconnected student database (IRB-1) at their respective university and then upload, in near real-time that data into a single database (IRB-2) associated with the Department of Emergency Medicine. Such a linked dataset would enable the tracking of diseases and injury while also allowing for more rapid warnings pertaining to the emergence of new disease and injury.
This big idea has been set in motion, a pilot launch was trialed, and the need for such a comprehensive de-identified student dataset is recognized. The limitation is funding for a dedicated programmer to both expand on the development of UVA’s existing database (IRB-2) and to assist the other participating universities with the creation of their datasets (IRB-1) and the uploading of their de-identified data. The current Department of Emergency Medicine team associated with this project is working in a multi-disciplinary manner with faculty from various UVA schools and the Division of Student Affairs. This team has been engaged with numerous student researchers who worked on projects associated with UVA data (IRB-1), with the potential for numerous future studies with a national dataset (IRB-2). This concept has the potential, as a multi-site project, to raise significant future funding from both grants and industry (similar to the NPDS) and have significant impact on the student population. In order to launch this bold idea, seed funding is needed for a programmer who is dedicated to this project and who is acquainted with all higher education datasets listed above in the IRB-1 dataset and familiar with the current IRB-2 dataset. A dedicated data scientist is also needed to assist with the de-identified data. This concept is feasible and would be groundbreaking nationally, positioning UVA as the leader in research pertaining to students presenting to the emergency department and other entities associated with the nation’s universities.
Funding Request: $250,000 we cannot pay salary from donated funds
-
- This trainer will allow our department to teach students and residents the skill of arterial line placement. This procedure is used in our most critically ill patients and provides intensive monitoring of hemodynamics and blood pressure. The procedure is more successful with ultrasound guidance, which this trainer also facilitates.
-
- This trainer will allow our department to teach students and residents the skill of central line placement. This procedure involves placing a more durable and robust line in the central venous system for vascular access. This facilitates the infusion of life saving therapies such as antibiotics, fluids, and blood products as needed. This procedure has been shown to be safer and more successful with ultrasound guidance, which this trainer facilitates.
-
- This trainer will allow our department to teach students and residents the skill of arthrocentesis. This procedure involves inserting a needle into a joint space for diagnostic or therapeutic purposes. In emergency medicine, we often perform this procedure to obtain joint fluid for laboratory analysis in order to evaluate for infection. The simulator allows for ultrasound guidance of the needle into the joint space, which has been shown to be more effective and result in fewer needlesticks for the patient.
- Ultrasound guided needle trainer(approximately $50,000)
-
- This is an exceptionally robust ultrasound simulator that allows for student and resident instruction of nearly any ultrasound guided procedure. More and more procedures have been shown to benefit from active guidance of the needle under ultrasound imaging. This allows for the physician to see the needle at all times during a procedure and avoid inadvertent needle puncture into non-targeted objects and anatomy. This particular trainer allows for simulated guidance of needle guided procedures in a very high fidelity format.
-
- This is a question bank that could be used for our two current emergency ultrasound fellows to prepare themselves for the board certification test in advanced emergency ultrasound.
