Pulmonary & Critical Care Fellowship
Message from the Program Director
Thank you for reviewing our website and showing interest in our training program. Our top priority is the professional development of our fellows. This consists of extensive education in the core principles of pulmonary and critical care medicine and individualization of training to match our fellows’ unique interests.
Dr. Cathy Bonham and I have collectively over 20 years of experience in PCCM fellowship education. We appreciate that there are many paths open to our trainees.
Our Program’s Mission Statement is as follows: “We strive for excellence in the care of our patients, ourselves, and our community.”
We live this statement through our Core Values.
- Patient and fellow safety come first!
- We are committed to a culture of excellence. We make ourselves accountable. We strive to do the right thing for the right reason, at the right time, and in the right way.
- We are committed to our fellows’ professional development.
- We believe in collaborative leadership.
Please look around the website and review our clinical rotations, conferences, and research opportunities. Also, review the biographies of our current faculty and fellows and past fellows. We are certainly happy to answer any additional questions you may have about the program.
We hope you will consider applying to our program, and we look forward to hearing from you.
Sincerely,
Timothy J. Scialla

Timothy Scialla MD
Pulmonary & Critical Care Fellowship Program Director

Catherine Bonham MD
Pulmonary & Critical Care Associate Fellowship Director

Taylor Lloyd
Pulmonary & Critical Care Fellowship Education Coordinator
Program Overview
The Pulmonary and Critical Care Fellowship at the University of Virginia is a three-year program that provides a robust background in clinical pulmonary medicine and managing critically ill patients.
We provide strong mentorship for professional development during fellowship. There are opportunities for fellows to stay for an additional year of training. This additional year is specifically encouraged for those who want to pursue a grant-funded clinical investigator career or a combined fellowship, such as with clinical informatics. Fellows can tailor the experience based on their interests.
| Typical PCCM Fellowship Schedule (weeks) | Year One | Year Two | Year Three |
|---|---|---|---|
| Orientation | 3 | 0 | 0 |
| Medical Procedures | 1 | 0 | 0 |
| Medical ICU Days | 13 | 8 | 5 |
| Medical ICU Nights | 4 | 4 | 5 |
| Medical ICU Education | 2 | 2 | 2 |
| Pulmonary Consultation Service | 9 | 4 | 0 |
| PFTs and Sleep | 4 | 0 | 2 |
| Interventional Pulmonary | 4 | 4 | 4 |
| Research and Clinical Elective | 3 | 30 | 16 |
| Subspecialty Pulmonary Clinics | 3 | 0 | 4 |
| Thoracic and Cardiac Surgery ICU | 4 | 0 | 0 |
| Neurologic ICU | 0 | 0 | 4 |
| Coronary Care Unit | 0 | 0 | 4 |
| Lung Transplant | 4 | 0 | 4 |
| General Pulmonary Continuity Clinic 1/2 day per week | |||

PCCM fellows ready to learn
After completing their fellowship, fellows are eligible to take the American Board of Internal Medicine’s Pulmonary Medicine and Critical Care Medicine examinations.
Roughly half of our graduates go into academic positions, and the other half go into private practice. See where fellows go here.

PCCM fellows ready to learn
Pulmonary and Critical Care Fellowship program goals:
- Develop fellows’ competencies in the specialty of pulmonary disease through a comprehensive training experience in which they encounter and treat a broad spectrum of patients with pulmonary disease in both hospital and outpatient settings and in close collaboration with division faculty. In addition to an ambulatory continuity clinic, fellows rotate through the pulmonary subspecialty clinics and outpatient clinical electives.
- Develop fellows’ competencies in the specialty of critical care medicine. While most of the critical care experience is in the Medical Intensive Care Unit, each fellow rotates through non-medical intensive care units as well. Fellows lead our medical ICU teams in collaboration with our faculty, developing competencies across a broad spectrum of diseases.
- Develop fellows’ competencies in research methodology, scientific literature appraisal, and evidence-based clinical decision-making. Fellows engage in mentored research and scholarly activities during their second and third years with the aim of developing professional skills as a clinician-educator or clinician-scientist. Development of clinical expertise complementary to the academic focus is encouraged. Fellows’ ability to communicate effectively is strengthened through presentations and manuscript writing in a collaborative environment with mentors and interdisciplinary teams.
Pulmonary Consultation Service
Fellows spend at least four months providing consultation services. Patients from the medical, surgical, neurologic, and obstetric units are seen, including critically ill patients in the surgical and neurological intensive care units (ICUs) and the cardiac care unit. The fellows perform bronchoscopies, thoracentesis, and chest tube insertions under the supervision of the attending physician. Emphasis is placed on the fellow’s professional development into an expert in inpatient pulmonary consultation. The fellow consultant develops proficient skills in:

Pulmonary Consultation service in action on Fancy Dress Friday!
- Medical knowledge
- Patient communication
- Interprofessional communication (chest radiology and primary teams)
- Documentation
- Coordination of care
- Proper triage
Fellows on this service work 6 days per week with Sunday off. The typical work hours are 7:00 a.m. to 5:00 p.m., Monday through Friday, and 8:00 a.m. to 2:00 p.m. on Saturdays. The fellow signs the pager over to the night covering fellow each night, ensuring no clinical responsibilities outside of the hospital hours. (56hrs/week)
Interventional Pulmonary Rotation
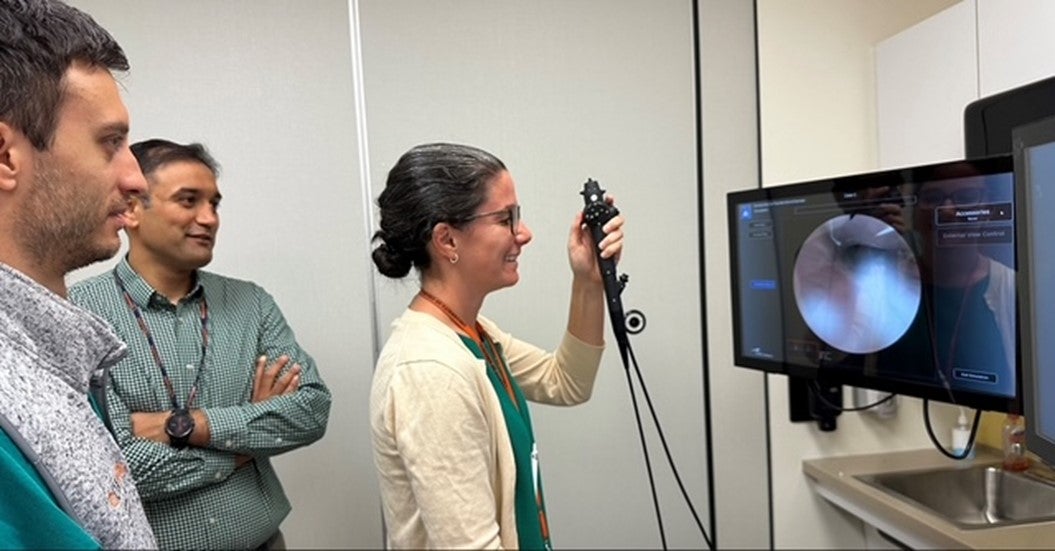
First-year fellows using our Bronchoscopy simulator with IP attending Dr. Subodh Pandey.
In addition to advanced bronchoscopy and pleural procedures that may occur during other rotations, fellows spend a month each year as a dedicated fellow alongside our three fellowship-trained interventional pulmonology (IP) attending physicians. In this capacity, our fellows are immersed in the IP during this rotation, receiving ample one-on-one training in:
- Endobronchial ultrasound (EBUS) bronchoscopy
- Robotic bronchoscopy
- Airway stenting
- Ablation techniques
- Advanced pleural procedures
UVA IP Section Chief Ellen Volker, MD, MSPH, teaching Friday fellows’ session. Dr. Volker has co-directed the national AIPPD robotic bronchoscopy course and oversees the IP curriculum for our PCCM fellows.
This rotation enables our fellows to acquire proficiency in advanced bronchoscopic techniques, which are the cornerstone of a pulmonary specialist’s practice that includes bronchoscopy.
Procedures are performed in the intensive care units, UVA operating room, and the multidisciplinary endoscopy unit. Fellows interested in IP careers can perform additional electives.
In addition, our fellows participate in the IP clinic. This affords them exposure to patients with complex abnormal chest imaging under the apprenticeship of expert instructors.
Fellows on this service work five days a week. Weekends are off, and there are no clinical duties outside of work hours. The typical work hours are 7:00 a.m. to 7:00 p.m., although this schedule varies depending on the number of operating room (OR) cases. (60 hours/week)
Intensive Care Units

Fellow Naima Farah, Fellow Ibrar Islam, IP attending and mentor Subodh Pandey pose with the Bronschoscopic Lung Volume Reduction team in service of patients with advanced COPD.
Fellows spend at least six months in the medical ICU, where they evaluate and treat common and unusual cases under the guidance of the critical care medicine board-certified attending faculty. As a part of their daily responsibilities, fellows are expected to:
- Organize and lead teaching and work rounds.
- Formulate care plans with attending supervision.
- Facilitate communication among the ICU team, surgical services, consultative services, and family members.
- Perform and/or supervise critical care procedures.
Extensive experience is gained in:
- Ventilator management
- Hemodynamic monitoring techniques, including Swan-Ganz balloon flotation and arterial catheter placement
- Intubation
- Ultrasound-guided central venous catheter insertion
- Chest tube thoracostomy
- Percutaneous tracheostomy
- Emphasis is also placed on critical care ultrasound
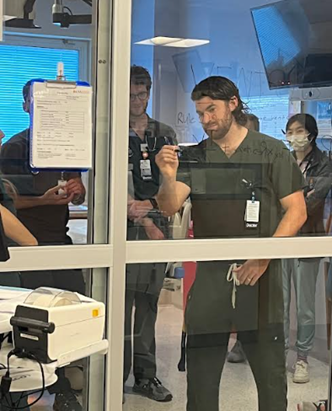
PCCM fellow Matt Freedman teaching ventilator waveforms to the MICU resident teams.
Rotations broaden the critical care experience through non-medical intensive care units, including time spent in:
- Thoracic and Cardiac Surgery Intensive Care Unit (TCV)
- Neurologic Intensive Care Unit
- Coronary Care Unit
In these units, pulmonary fellows care for patients who present with trauma, postoperative complications, strokes, spinal cord injury, cardiovascular diseases, or who are on ECMO.
Fellows on the MICU rotation work 6 days per week with one weekend day off. They are on call 4 days per week (7:00 a.m. to 7:00 p.m.) and on the other two days, they complete non-call day responsibilities (8:00 a.m. to 3:00 p.m.). After signing out in the afternoon or evening, fellows have no clinical duties outside of the hospital. (62hrs/week)
On non-MICU critical care rotations, fellows work 5 days per week and maintain one morning of ambulatory clinic. Weekends are off. Typical work hours are 8:00 a.m. to 4:00 p.m. (40 hours/week)
Outpatient Pulmonary Clinic

PD Tim Scialla and senior fellow Ibrar Islam in the continuity clinic. Who has the better pants?

Clinic attending Katie Waybill, MD, makes creative use of natural light to read an old film with fellow Caroline Chessare, MD!
Pulmonary fellows “on average” have a one-half-day continuity clinic weekly, seeing two new and several returning patients. Fellows follow their patients throughout the three-year fellowship. The fellows’ clinics are staffed by one of the Pulmonary/Critical Care attendings, specifically trained to supervise the fellows’ outpatient clinic. The senior fellows staff an Urgent Friday ambulatory clinic that focuses on patients of fellows who require more urgent or hospital follow-ups. During the PFTs and Sleep rotation, fellows are in the continuity clinic for two half-day sessions.
Clinics Rotation
The Clinics Rotation is a pure outpatient rotation that offers additional exposure to complex and rare pulmonary disease management through subspecialty pulmonary clinics, including those for cystic fibrosis (CF) and non-CF bronchiectasis, severe asthma, Advanced Chronic Obstructive pulmonary disease (COPD), Pulmonary Hypertension, interstitial lung disease (ILD), and Sarcoidosis.
Our subspecialty pulmonary programs have earned numerous accreditations for their multidisciplinary expertise in transforming patient care. Our pulmonary faculty is excited to share their experience with fellows.
- Joint Commission Certified Center of Excellence for Advanced COPD Care
- Cystic Fibrosis Foundation Accredited Adult and Pediatric Cystic Fibrosis Care Center
- Pulmonary Hypertension Association Accredited Clinical Center of Excellence
- Pulmonary Fibrosis Foundation Accredited Center of Excellence
- World Association for Sarcoidosis and Other Granulomatous Disorders Accredited Center of Excellence
- Bronchiectasis and NTM Care Center Network
- Lymphangioleiomyomatosis Foundation Approved Clinic
Fellows on the Clinics rotation work five days a week with no weekend or overnight clinical duties. The typical work hours are from 8:00 a.m. to 5:00 p.m. (45 hours/week)
Lung Transplant

Fellow Daisy Zhu, MD, UVA Lung Transplant Director, and mentor Hannah Mannem, MD and pharmacy resident Haley attending the International Society for Heart and Lung Transplant
UVA is proud to be the first lung transplant program established in Virginia in 1990 and remains the largest in the state. The fellows spend nearly two months on lung transplant rotation, seeing patients in all stages of the transplant process. This includes those undergoing evaluation for transplant, listed and waiting for a transplant, and recent and long-term post-operative patients. The emphasis of this rotation is to provide balanced exposure to both outpatient clinics and inpatient transplant services. There is also an opportunity to perform a transplant bronchoscopy, including a transbronchial biopsy, which, in the era of advanced and navigational bronchoscopy, has become less common in training programs.
Fellows on this rotation work five days a week, with weekends and evenings free from clinical duties. The typical workday is from 8:00 a.m. to 4:00 p.m. (40 hours/week)
Anesthesiology Elective
Starting in the first year, fellows perform airway management and intubation on all patients in the MICU. In the second and third years, the Pulmonary/Critical Care fellows can rotate to the Anesthesiology Service, where they can achieve additional proficiency in airway management and anesthesia critical care.
Fellows on this rotation work five days a week, with weekends and evenings free from clinical duties. The typical workday is from 8:00 a.m. to 4:00 p.m. (40 hours/week)
Pulmonary Hypertension Elective
In the final year of fellowship training, interested fellows can take a four-week elective in pulmonary hypertension with Dr. Andrew Mihalek, who directs our Pulmonary Hypertension Center of Excellence. It involves both an inpatient and outpatient pulmonary hypertension experience. It also includes dedicated time working with ECHO technicians in the hospital and reading room time with cardiology faculty, who review ECHOs. There is an opportunity to spend time in Nuclear Medicine reading V/Q scans. Finally, Dr. Mihalek performs RHCs on Fridays, and the fellow assists with these procedures.
Fellows on this rotation work five days a week, with weekends and evenings free from clinical duties. The typical workday is from 8:00 a.m. to 4:00 p.m. (40 hours/week)
PFT Rotation
A clinical physiology rotation is a unique opportunity to learn the foundations of pulmonary function testing under expert supervision. Rotations such as these were once commonplace in pulmonary fellowships. However, increasing service needs and a general de-emphasis of physiology have led to their dropping from programs. We aim to provide our fellows with this exposure because we believe a solid understanding of pulmonary physiology remains essential for comprehending the effects of disease, and that pathophysiology bridges cellular events and the patient’s experience.
This rotation requires extensive outside reading on the part of the fellow in addition to providing hands-on training in:
- Pulmonary function
- Exercise testing
- Laboratory management
- Quality control
The fellows will also meet individually with attendings who have a background in physiology and pulmonary function testing. These meetings will review the pulmonary function testing and provide an opportunity to discuss various physiology topics.
Sleep Medicine
Board-certified sleep medicine faculty guide fellows through this introduction to the fundamentals of sleep medicine. The rotation includes activities at the Sleep Disorders Center with its associated Sleep Lab. Although sleep apnea syndromes make up a large part of the caseload, all types of sleep disorders are seen during a clinic in this rotation. Ongoing research, particularly in the treatment of obstructive sleep apnea, is discussed. Pulmonary fellows gain experience in patient evaluation and the techniques and interpretation of nocturnal polysomnography.
Fellows on this rotation work 5 days per week, with weekends and evenings without clinical duties. The typical workday is from 8:00 a.m. to 4:00 p.m. (40 hours/week)
MICU Night Rotation
Fellows spend one month annually as the MICU night fellow, divided into one-week blocks throughout each year. Night rotations have become increasingly common in PCCM programs as a more effective alternative to home calls. The structure of this rotation and others ensures that no UVA PCCM fellow has 24 consecutive 24-hour calls, and we strictly adhere to ACGME day-off policies. We monitor all rotations closely annually for fatigue.
MICU Nights is one of our most popular rotations because of the autonomy and leadership it entails. The fellow covers the MICU resident teams and leads the admission of new patients overnight to those teams. There is an in-house MICU intensivist attending to provide supervision throughout the entire evening. The fellow leads nurse work rounds, transfer calls, and MICU triage.
This is a demanding rotation, and fellows work seven consecutive nights, bookended by 48 hours off clinical duties.
Global Health Curriculum and Elective
This curriculum was developed by one of our fellows. Its overarching goal is to expose interested fellows to the complexities surrounding global health practice, research, education, and policy in the context of anesthesia, pulmonary medicine, and intensive care. Phase 1 of the curriculum involves active participation in the Global Health Journal Club sponsored by the Division of Infectious Diseases and the Department of Anesthesia. This is open to all our fellows. For those who would like to make Global Health the focus of their research, Phase 2 involves identifying a mentor in Global Health and actively participating in their team meetings and research with that mentor. Those fellows who participate in Phases 1 and 2 can travel to a partner site in Rwanda, South Africa, or Tanzania for four weeks to foster cultural exchange and bidirectional learning.
Goals for Training
The overall goals of the research curriculum are to provide a meaningful, supervised research experience with protected time for each fellow, while maintaining essential clinical experience. Unless there are specific reasons, in general, the duration of this rotation will not exceed 12 months, such that the fellow can devote 24 months of the fellowship to clinical experience. Because fellowship clinical duties and assignments are more intensive in the earlier months of training, the research curriculum is designed to accommodate clinical training and set attainable but progressive research goals for each year of training.
Examples of recent research efforts by fellows with senior PCCM mentors include:
- Examination of the genomics of fibrotic lung disease and short telomeres
- Pulmonary MRI abnormalities in COPD
- Innate immunity in patients with asthma
- Development of a novel ‘flipped classroom’ educational curriculum for fellows
- Development of an Ultrasound curriculum for medical residency.
- Clinical Informatics ICU Bundle Board Design and Implementation
- Examining the impact of travel distance on pulmonary outcomes in patients with sarcoidosis
Year 1 – Foundational Research and Clinical Integration
Research Goal: Identify a primary mentor and define a research question with preliminary data collection or study design development.
Milestones:
- Confirm primary mentor by the end of Research Week.
- Formulate research question by February.
- Present early-stage project proposal at Grand Rounds.
- Confirm mentorship committee selection and set the first meeting by May.
- Submit IRB application (if applicable) by the end of Year 1.
Year 2 – Intermediate Research Development and Conference Presentation
Research Goal: Conduct data collection, develop an abstract, and present at a national specialty meeting (e.g., ATS).
Milestones:
- Submit conference abstract by fall.
- Present findings at a national meeting (e.g., ATS).
- Refine data analysis and manuscript outline.
Year 3 – Research Completion and Scholarly Dissemination
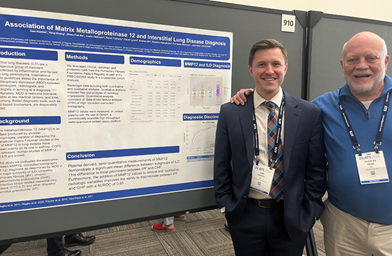
Sam Konkol presenting his Poster at ATS in San Diego.
Milestones:
- Submit manuscript to a peer-reviewed journal.
- Present the finalized project at an institutional or national conference.
- Develop a long-term career plan that integrates future research opportunities.
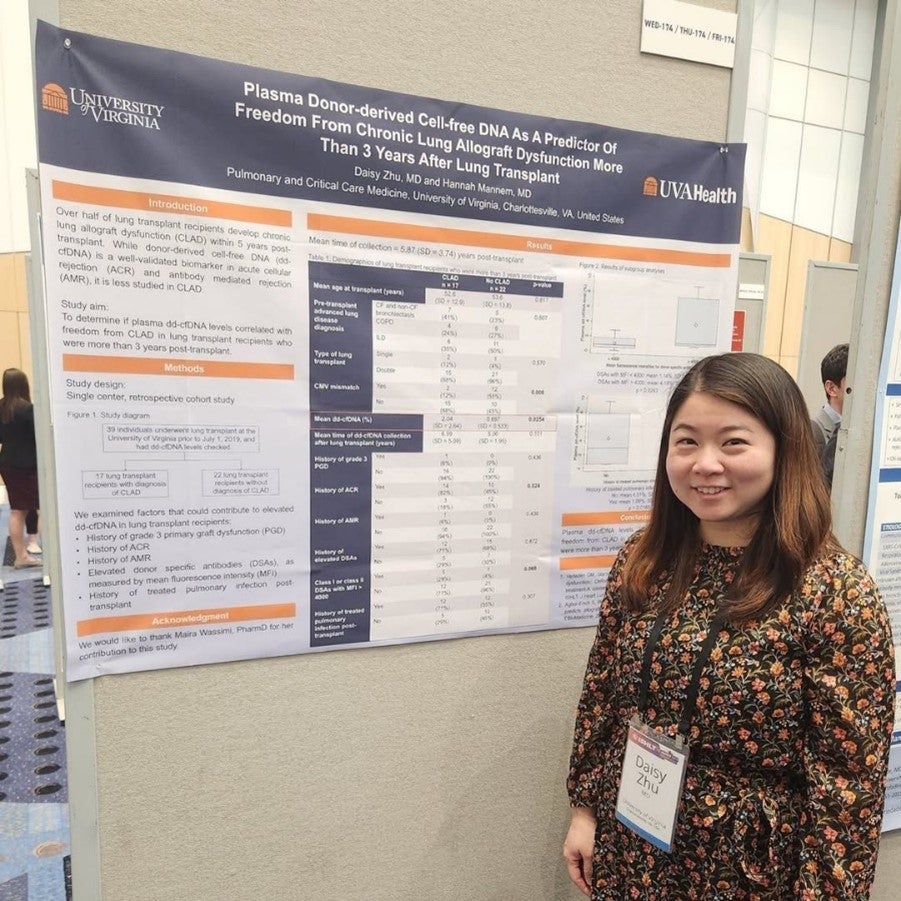
Daisy Zhu presents her lung transplant research at ISHLT
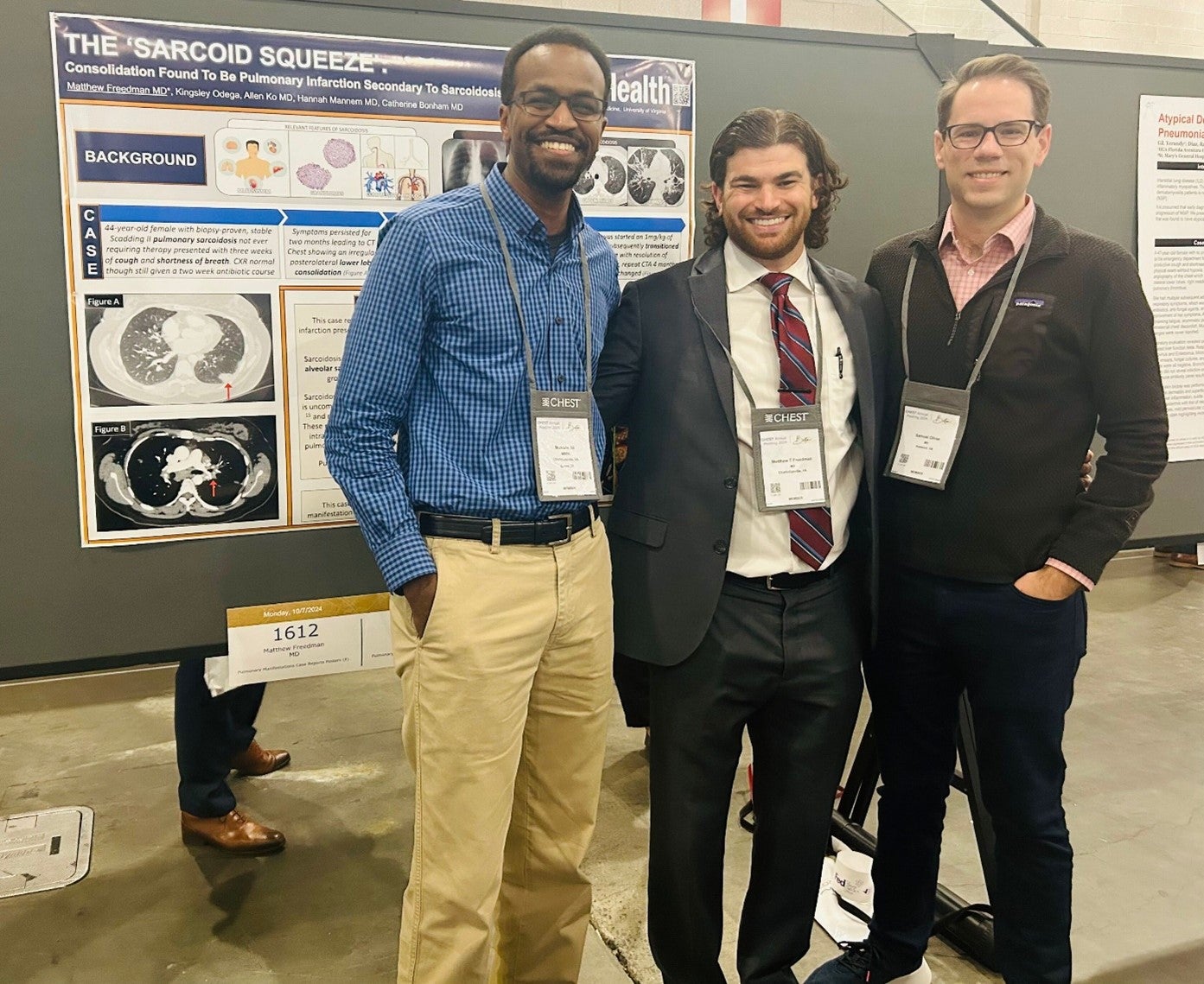
Matt Freedman presenting at CHEST with Mustafa and Sam giving fellowship support.

UVA PCCM Division spending time together at ATS 2025
Pulmonary Grand Rounds

Our Fellows meeting with PGR guest speaker Wes Ely, MD.
Designed to focus on topics in pulmonary and critical care medicine in which management and research are actively evolving. Our faculty and invited speakers from throughout the department and the School of Medicine present such topics weekly. We also have guest speakers from outside the institution who are experts in their respective fields. Fellows are invited to meet with these guests to expand their contacts and initiate networking. We also have our fellows present their research in progress at Pulmonary Grand Rounds. This conference is held at noon on Mondays from September through May.
Chest Imaging Conferences
This bi-monthly conference highlights interesting and challenging cases on the pulmonary consultative service. Fellows gain experience in interpreting unknown chest radiographs. The conferences are moderated by faculty members committed to education and clinical reasoning. In response to feedback, we have invited a chest radiologist to this conference, which has been a great addition. Furthermore, we have begun to incorporate didactics on CT imaging and interpretation, led by our Chest Radiologist. This conference takes place on Mondays at 1:00 p.m., immediately following PGR.
Ultrasound Conference
This conference is also held bimonthly and includes both didactics on US techniques and interpretation, as well as a review of fellow-acquired images from the MICU. The expectation is that the skills and content discussed in this conference are practiced at the bedside by fellows under direct supervision from both faculty and more senior fellows.
Didactic Lecture Series
This series covers core topics in pulmonary and critical care medicine. It is offered bimonthly as a two-hour conference on Fridays immediately following Medical Grand Rounds. This format has allowed our lecturers and fellows to delve deeper into complex pulmonary and critical care issues that cannot be covered in a one-hour session. Due to the bimonthly scheduling, we also ensure that all fellows can attend the two-hour session with their services fully covered by the attending physicians.
Quarterly Skills Days
The skills days are two-hour afternoon sessions that occur at least once per quarter and focus on high-yield areas of critical care medicine. They are led by expert faculty from inside and outside the division. In the past year, topics included a cricothyroidotomy lab, Blakemore tube placement, hands-on experience with ECMO circuits and cannulae, and a difficult airway skills session.
Pulmonary and Critical Care Medicine Journal Club

Critical Care Medicine Journal Club in Session!
In this weekly journal club, faculty and fellows present recent articles that provide up-to-date outcomes studies in critical care medicine, developing the fellow’s skills in critically interpreting the literature. Emphasis is placed on breakout articles that will immediately impact the field, as well as various studies covering different study designs. We also include “classic articles” so that fellows can read the primary literature that has become practice-changing. The CCM JC occurs on Wednesday at noon in the MICU conference room.
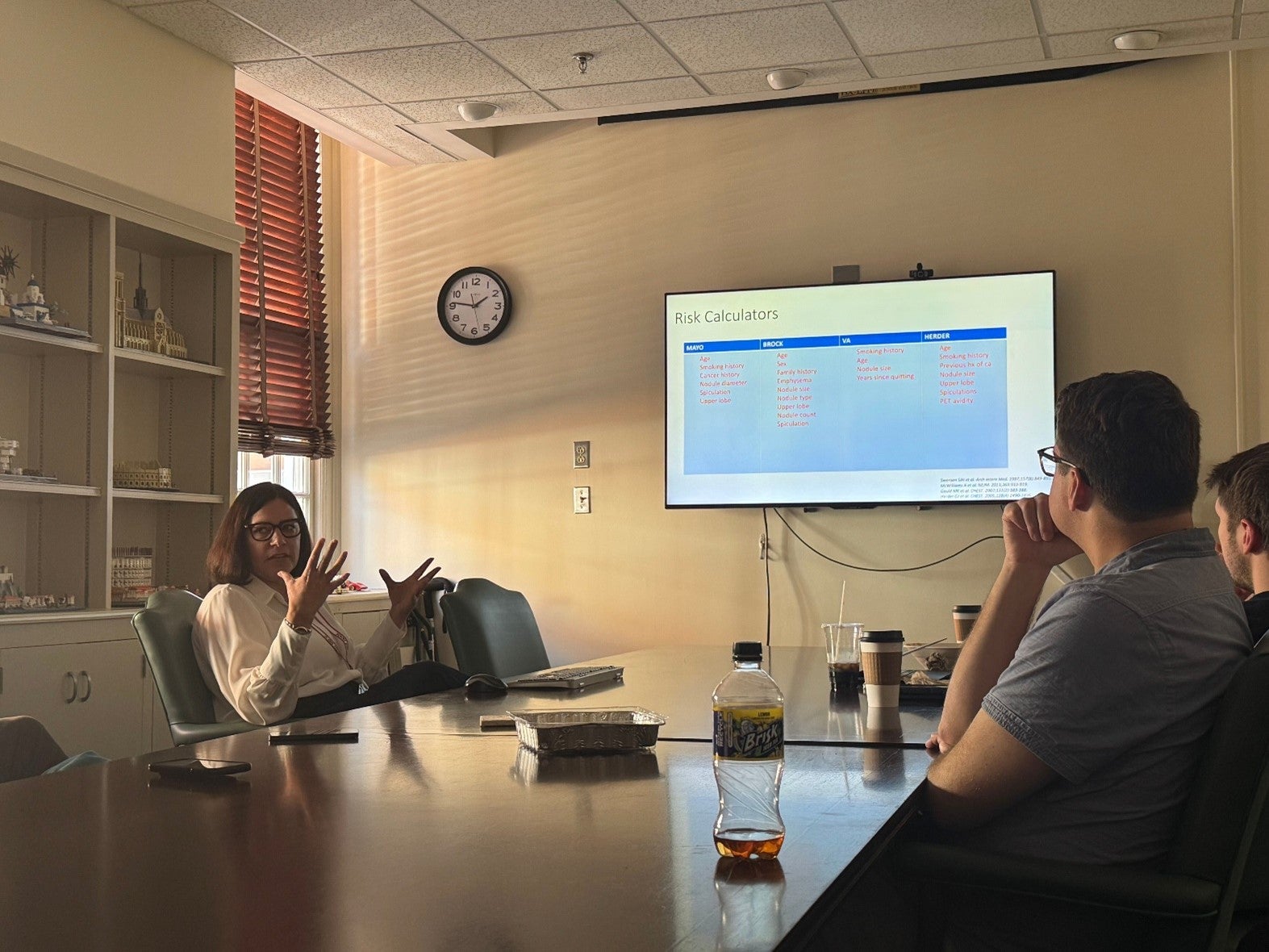
Ambulatory Conference
A popular recent addition to our conferences has been the Ambulatory Conferences, which occur immediately following the Continuity Clinic on Thursday mornings. The conference utilizes the teaching scripts created by the APCCMPD teaching series for these sessions. We also review recent relevant journal articles in pulmonary medicine.
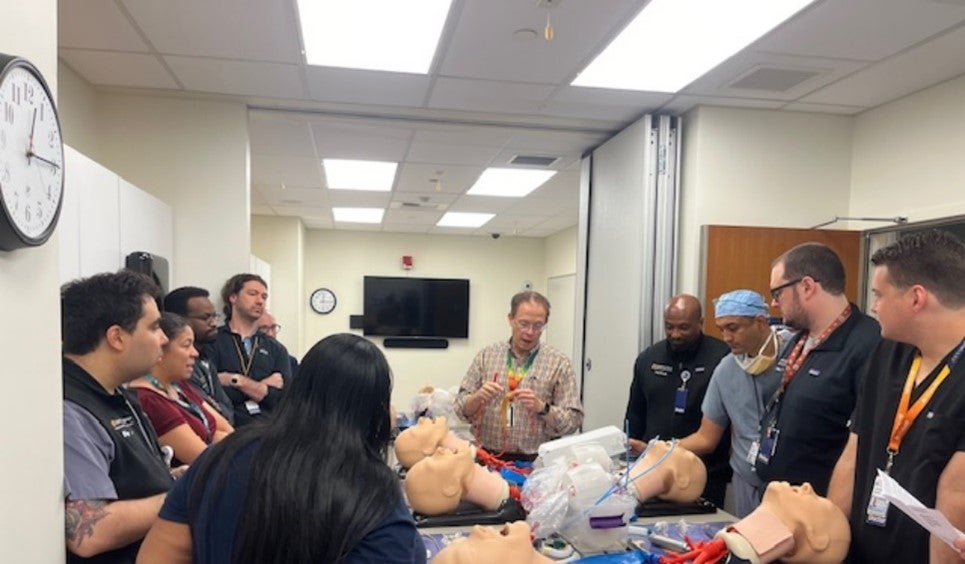
Drs. Enfield and Pandey guiding fellows on proper technique and steps for Blakemore Tube placement.
ILD Multidisciplinary Conference
Fellows and attendings meet via ZOOM in a multidisciplinary format with members of the Pathology and Radiology Department to review complex cases of diffuse parenchymal lung disease. The conference structure promotes a multidisciplinary dialogue focusing on ILD, lung cancer, and other disease processes. This is a bi-monthly conference that takes place on Thursdays at 4:00 p.m.
MICU/QI Conference
This monthly conference brings together members of the MICU team, quality assurance leadership, and hospital team members to review quality assurance issues in the MICU, pulmonary service, and other related fields. The fellows learn skills related to quality assurance assessment and participate in systems analyses of patient outcomes.
Research Week
Research week occurs as a week of protected time amid the first year, typically in late January, during which each class works together as a group. It is a chance to discuss career development goals and solidify scholarly interests that develop during the first immersive clinical period of fellowship. Topics discussed include:
- Building a Mentorship Team
- Faculty research interests and projects
- Library and data resources
- CV and Biosketch development
- Project Proposal Development Workshop
At the end of the week, first-year fellows present a ‘mini-proposal’ of an area of mentored study they would like to engage in over the next two years.

Dr. Bonham leading Research Week with eager fellows.
See information on salary and benefits on the GME website.
Fellow wellness is a top priority of our program and is a factor in all decisions related to the fellowship program. There is an abundance of resources available. See information on GME well-being resources and learn more about the Faculty and Employee Assistance Program.
Introducing Pathways to Our Program
We have developed the following pathways that fellows may utilize as roadmaps to guiding their professional development when they have identified specific interests.
Clinician investigators are those individuals with an interest in having grant-funded research and peer-reviewed publication as cornerstones (more than 50%) of their future faculty career. The interested applicant should be committed to a fourth year of training focused on research, or have extensive prior research training and experience (Masters or PhD level). A fourth-year student is funded by training grants internal to UVA or by obtaining external support via an NIH F32 or similar early-career development foundation grants. The division has a track record of success in preparing fellows for this pathway.
A typical timeline would be as follows:
- At the time of interview/program recruitment, the interested applicant would notify the program that they wish to pursue the investigator pathway if matched to our program. These applicants will undergo a second review of their ERAS application by our research leadership to ensure the candidate meets our program’s criteria. Applicants would then be notified before the match if we would support the CI pathway if they match with our program.
- The first year would be similar to all other fellows with clinical rotations and three weeks of research elective time (including Research Week).
- The first six months of the second year would be focused on research time to develop data for an early career development award submission (December of the second year). If not awarded, the candidate will prepare for resubmission in April of the second year.
- In the second year, the mentor and mentee would pursue internal training grants with the aid of division leadership.
- A total of 18 months will be dedicated to trainee research in the 36-month program in the first three years.
- A fourth year entirely devoted to research without clinical duties of the fellowship, unless requested by the fellow to maintain clinical skills.
Goals, Objectives, Outcomes
This 24-month track will support fellows in gaining the knowledge, skills, and methods necessary to become leaders in healthcare systems’ quality and safety committees, initiatives, and prepare them for careers in this field.
Learning Objectives
- To obtain knowledge of quality improvement methods
- To apply quality improvement methods to a healthcare gap in quality
- To identify system failures and medical errors in health systems and report them in the appropriate hospital error reporting system.
Outcomes
Upon completion of this pathway, fellows will be awarded a certificate of completion and graduate with a distinction in Quality and Process Improvement and Patient Safety, as well as a Lean Six Sigma Healthcare Green Belt.
Learning, Courses
Online learning
- Stanford Medical Statistics Program, one year course
- Basic Certificate in Quality and Safety from the Institute for Healthcare
Improvement - Lean Six Sigma Healthcare Green Belt
- Coursera Patient Safety Specialization
- EPIC Physician SmartUser Course; Optional to do other Epic Physician
Builder Courses
Experiential Learning
- Teaching Experience (Optional): Mentorship in UVA IM Quality Improvement Didactics (Jessica Dreicer)
- Committee Membership:
- Attend MICU (or alternative) Unit-Based Leadership meeting weekly (Thursdays 2-3)
- Attend Critical Care Subcommittee Meetings
- Participate in at least one morbidity or mortality meeting (sharps, sepsis, etc.)
- Review requests for changes, research proposals
- Offer clinical expertise to the Data Science Group
- Participate in a QI project linked to a clinical site’s quality improvement goals.
- Poster presentation at SCCM, ATS, UVA Health QIPS Showcase, or Virginia Patient Safety Summit
Proposed Schedule
| Year 1 | Apply for the track
Develop a potential QPI project that aligns with unit-based goals and is approved by PCCM leadership |
| Year 2
(FALL) |
PHS 7365- LEAN for Healthcare, with Dr. Wendy Novicoff
Coursera Patient Safety Specialization Committee participation Capstone project start |
| Year 2
(SPRING) |
Coursera Patient Safety Specialization
Committee participation Capstone project continues |
| Year 3
(FALL) |
Stanford Medical Statistics Program
PHS 7450- Informatics: Databases & Data Life Cycle Committee participation Capstone project continues |
| Year 3
(SPRING) |
Lean Six Sigma Healthcare Green Belt
Committee participation Poster/publication of the capstone project |
Application Process
Participation is restricted to PCCM fellows in their 2nd year or higher.
Two components:
- Personal statement describing commitment to the track, interests in QPI and Patient Safety, and personal goals. This should include an area of interest. Limited to no more than 1 page.
- Interview with Dr. Enfield. Dr. Scialla.
This pathway dedicates twelve months of research to medical education, which includes a longitudinal curriculum in Medical Education that emphasizes curriculum development. The pathway also allows the PCCM fellow to assist in the Pulmonary Module for second-year medical students, which takes place over three weeks. Fellows on this pathway take a larger role in designing and implementing the didactic curriculum for our program. There is also an emphasis on providing lectures to the IM residency program throughout the second and third years of training.
Each fellow interested in this pathway must identify a mentor within the division who focuses on medical education, as well as a mentoring team from outside the division that has roles in UME and/or GME. Each fellow on this pathway is responsible for a CAPSTONE project in developing a curriculum in year two and then implementing the curriculum, if feasible, in year three. Through sponsorship from the mentor and the mentoring team, the fellow is encouraged to participate in educational committees at both the regional and national levels, including those affiliated with CHEST, ATS, or the APCCMPD.
The final component of this pathway is to identify a clinically focused area of specialization at the sub-specialty level (e.g., CF, Pulmonary HTN, ARDS, COPD, Asthma) to become a content expert. This can include adding a subspecialty clinic during the second and third year and conducting smaller research projects in the field of interest.
Application Information
We sincerely appreciate your interest in our program.
For interviews for the 2025-26 fellowship selection cycle, UVA is following AAMC guidance and will conduct virtual interviews for all applicants. Depending on interests, we have hosted an in-person “second-look” that follows our rank list meeting.
We understand that AI tools can assist applicants in improving their applications by enhancing clarity and checking for grammar mistakes. Please be mindful of your authenticity and use AI tools to enhance rather than replace your thoughts and experiences.
We do not require applicants to disclose the use of AI during our application or interview processes. We expect applicants to follow the specific guidelines provided by the application and match systems.
We elect not to use AI tools in our application review process. We have dedicated and trained faculty who utilize a holistic review process, considering all aspects of an applicant’s profile.
Planned Use of Program Signaling
While we preferentially review applicants who signal our program, we also consider applicants who do not.

Hike to nearby Humpback Rock.
The UVA Pulmonary and Critical Care Fellowship Program participates in the Electronic Residency Application Service (ERAS) and the National Resident Matching Program.
Applicants must have completed an accredited residency within the last five years.
Current UVA Health System Policy on Occupational Health: All current Team Members must be fully vaccinated with a COVID-19 vaccine listed on the World Health Organization (WHO) Emergency Use List (EUL). Team Members who are not fully vaccinated (including those who have been granted an exemption under the policy) must comply with all directives of the Hospital Epidemiologist, including testing, masking, etc. Please note that we are not asking for your vaccination status. Please do not send us your vaccine record. Should you match with us, that information will be collected during the onboarding process.
We sponsor J1 visas; however, we do not sponsor H1B visas. To be appointed as a resident or fellow, all graduates of international medical schools must hold a valid certificate issued by the Educational Commission for Foreign Medical Graduates (ECFMG), in accordance with the requirements of the ACGME and the VA Board of Medicine.
We do not currently offer a fellowship program in pulmonary medicine or critical care medicine.
Trainee appointment is conditional based on the approval of the Clinical Staff Credentials Committee (CSCC) and the Clinical Staff Executive Committee (CSEC) and based on successful completion of credentialing, including but not limited to our review and acceptance of information from the criminal background check, successful completion of the pre-employment drug screen, passing practical medical licensing exams, receipt of a Virginia Medical License (if applicable), honest and accurate completion of all required paperwork and training modules before Orientation. For more information, please refer to the sample GME Contract.
The online Application is a two-step process:
- Enter ERAS application information once open. Documents will be accepted from ERAS only.
- Submit your ERAS application to the specific institution of your choice (i.e., the University of Virginia). We begin reviewing applications on the third Wednesday in July, and interviews are completed by the end of October. Applications that are not fully submitted and complete by the fourth Friday of July will not be reviewed.
The following documents must be submitted to the ERAS system before we will evaluate your application:
- Common application form
- Personal statement
- Medical school transcript
- Three letters of recommendation (one from your program director and two others from your current institution)
- Wallet-sized color photograph
- ECFMG status report (foreign medical graduates only)
Contact Taylor Lloyd, Fellowship Coordinator, with questions:
Email – BHD5WG@uvahealth.org
Phone – 434-924-9610
