Blue Light Fluorescent Cystoscopy
About
Bladder cancer is the fifth most commonly diagnosed cancer in the US with an estimated 81,0000 new cases each year. Most of these cancers are found at an early stage, however, finding some early stage tumors and lesions may be challenging due to the inconsistent ability to distinguish them from healthy tissue when viewed through a scope only using white light, making these tumors more difficult to treat.
Today, patients have an additional option when undergoing a biopsy or surgical removal (called a resection) of a suspected or known bladder cancer. Urologic Oncology surgeons at UVA are now using Blue Light Cystoscopy with Cysview® (BLCC) to better diagnose, evaluate, and remove bladder cancer tumors and lesions. Clinical trials have shown this procedure to be so effective that it is included in the bladder cancer guidelines published by the American Urological Association (AUA) and the Society of Urological Oncology (SUO).
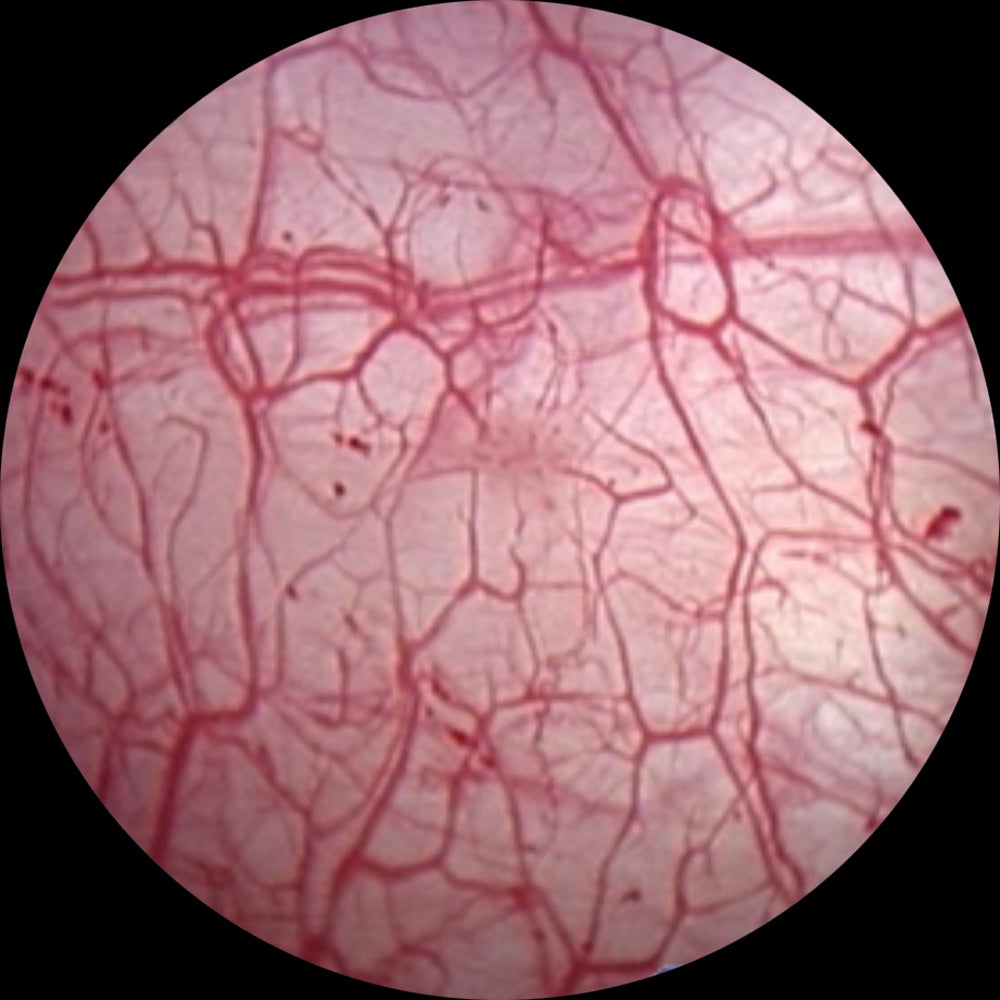
Bladder image using white-light cystoscopy alone
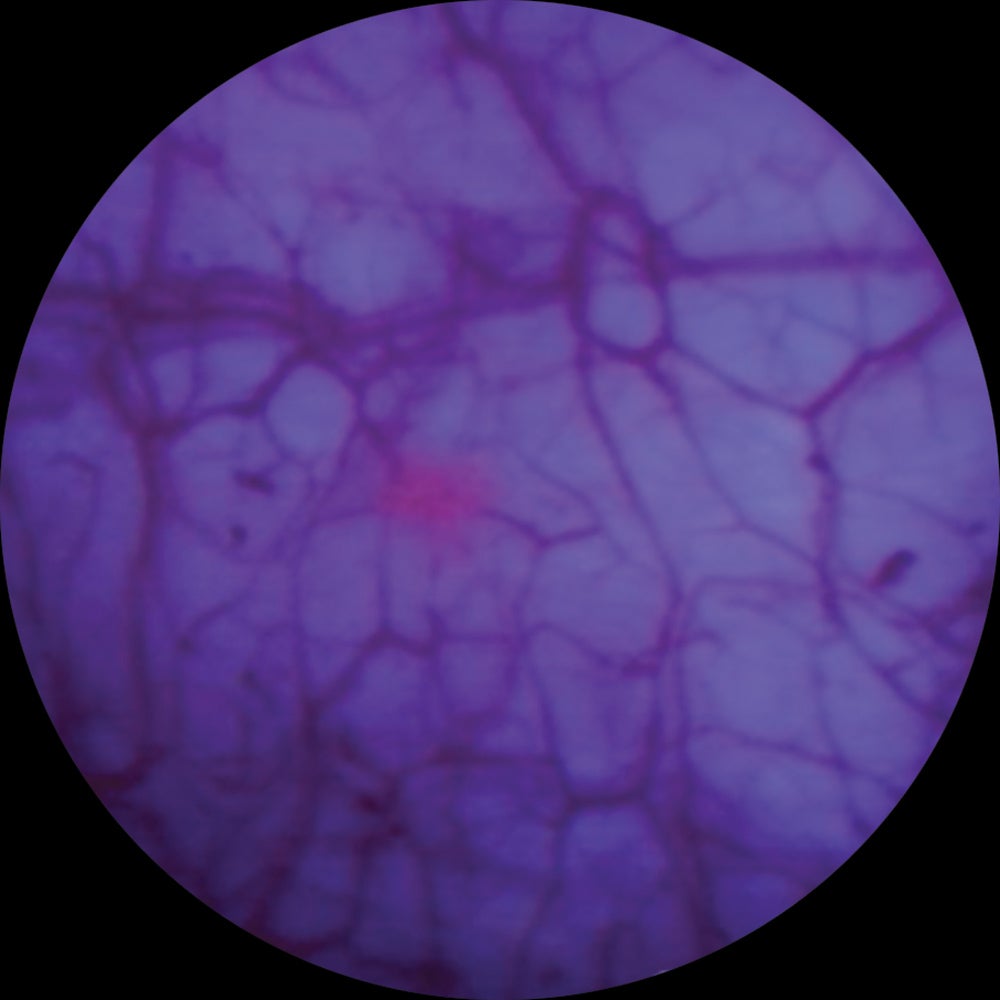
Same image using blue light Cystoscopy with Cysview as an adjunct to white light
Frequently Asked Questions
UVA Urology was the first facility in the state of Virginia to offer this procedure.
Patients seeking treatment for bladder cancer have many different choices on when it comes to where to go for their care. There are more diagnostic tools and treatments now than ever before. Blue Light Cystoscopy with Cysview is an important tool that can aid in the diagnosis and treatment of bladder cancer, and finding a center that offers this option can make a big difference. Below are the answers to some common questions about Blue Light Cystoscopy with Cysview, and bladder cancer detection and treatment.
In the earliest stages of bladder cancer, cancer cells are located on the surface layer of the bladder wall. Identifying this kind of cancer, which is called non-muscle invasive papillary bladder cancer (NMIBC), requires a correct and thorough work-up, and diagnosis is a key component of successful treatment.
To diagnose this disease, surgeons inspect the inside of the bladder using a long, thin tube called a cystoscope that includes a video camera on the end. In the past, the only option was white light cystoscopes, which do not always easily show tumors or cancerous lesions.
Blue Light Cystoscopy with Cysview (BLCC) uses a cystoscope equipped with both white and blue light for visual inspection inside the bladder. Cysview is a light-sensitive imaging drug called hexaminolevulinate (HAL) hydrochloride. BLCC may also be called fluorescence cystoscopy.
Medical staff begin by inserting a small amount of the Cysview solution into the bladder and cancer cells located in the superficial layers of the bladder, if present, begin absorbing the medication. The surgeon then uses a cystoscope using white light, to visualize the bladder wall, which may find larger, more easily apparent, tumors.
After switching the cystoscope to cast a blue light on the bladder wall, Cysview-infused tumors or lesions, including small ones, will appear in vivid pink, while the surrounding healthy tissue remains blue. The striking color differences help surgeons to detect, biopsy, and surgically remove just cancerous areas, while keeping healthy tissue intact.
Because only bladder cancer cells absorb the Cysview solution, the blue light mode allows the surgeons to visualize smaller tumors and lesions that may not be seen with a white light. The surgeon can immediately remove diseased tissue (called a resection), ideally leaving a clean margin of healthy tissue around it. BLCC has given urologic surgeons the ability to better evaluate, identify, and remove hard-to-see tumors more accurately and therefore further reducing the likelihood of recurrence if cancer cells are missed.
An enhanced visualization of smaller tumors and cancerous lesions of the bladder with BLCC allows for the option of resecting only cancerous tissue, therefore decreasing the need for a total cystectomy (removal of the entire bladder).
Physicians can repeat the Blue Light Cystoscopy more quickly after surgery or treatment than with white light cystoscopy. The Cysview solution shows cancer tissues as pink even if there is inflammation caused by surgery or treatment, which makes blue light an effective follow-up approach than a white light cystoscopy.
The short answer is: No.
Bladder cancer falls into two general categories:
- Non-muscle invasive bladder cancer (NMIBC): About 70 percent of all bladder cancers fall into this category, in which a tumor (also called a lesion) is still in the inner layer of cells of the bladder’s inside wall. Subtypes include Ta, carcinoma in situ (CIS) and T1 lesions.
- Muscle invasive bladder cancer (MIBC): This disease, which is less common than non-muscle invasive, occurs when the cancer has grown into deeper layers of the bladder wall. This disease is more likely to spread to other organs and is more difficult to treat. These cancers include the subtypes T2, T3, and T4.
BLCC readily detects the first type, NMIBC, which may be hard to distinguish from healthy tissue. Due to their more advanced nature, MIBC tumors are detected through white light cystoscopy, biopsies, a manual exam, imaging and other diagnostic tests.
BLCC is only effective at identifying non-muscle invasive bladder cancer. However, it is an additional tool that may improve accurate assessment and treatment of your disease. It is always used in conjunction with other diagnostic tools such as biopsies of suspicious and random tissues and imaging to help confirm the stage and grade of the bladder cancer.
There are several circumstances in which BLCC may be appropriate:
- Persistent symptoms along with a medical evaluation and urine tests that indicate bladder cancer may be present after the initial inspection with white light cystoscopy is negative.
- Treatment for non-muscle invasive bladder cancer (NMIBC) causes inflammation that interferes with standard white light cystoscopy.
- Doctors need to differentiate a diagnosis between NMIBC or more advanced muscle-invasive bladder cancer, each of which require different treatments.
- Surgeons need to check for a recurrence of bladder cancer after treatment.
As always, your physician will work with you to determine if BLCC is right for your particular case.
Clinical tests have shown that BLCC is safe and well-tolerated. However, no surgical procedure is free of any risk, so you should consult your doctor regarding the risks and benefits of this procedure for your individual circumstances.
Most people are ready to go home shortly after a routine procedure. However, this will depend on the extent of your disease and how much tissue may have been removed from your bladder. Your doctor will advise you on how much rest and care you will need afterward.
