Evaluation of Infertility
The Medical History
A thorough medical history is necessary for the successful diagnosis and treatment of male infertility as numerous potential causes exist which can impact sperm production. These may include genetic, congenital (born with), medical, sugical and environmental factors. Discussion of the duration of infertility, prior fertility treatments, previous preganicies and a detailed reproductive and sexual history is required.
Similarly, a review of past medical and surgical treatments, smoking and other drug use, and a family history are important in obtaining a complete picture of a couple’s health. The most efficient interview is undertaken with the couple together and we suggest bringing your partner to the appointment.
The Physical Examination
During your visit, you will have a physical examination performed which is important in assessing for additional causes of infertility. This includes examination of the penis, testes, epididymis, spermatic cord, and prostate. Each may have irregularities which can be associated with infertility. In some cases, an ultrasound may be required to further evaluate a suspected abnormality.
Semen Analysis
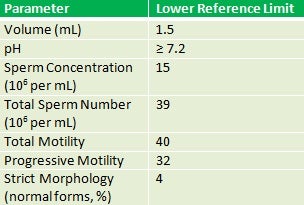
Table 1. 2010 WHO References for Semen Analyses
Two semen analyses are often indicated in the evaluation of male infertility as there can be variability in the results obtained from a single analysis. This is due to the large number of factors which impact sperm production and the length of a sperm cycle (approximately 70 days).
A semen analysis is not a perfect measure of fertility, but if abnormal, can suggest a diminished probability of achieving pregnancy. The semen is examined for the amount, consistency, number of sperm, movement of sperm, and sperm shape as well as other parameters. Reference ranges for semen analysis results have been previously established by the World Health Organization (see Table 1).
Please bring any prior semen analysis results to your visit. Keep in mind that not all laboratories specialize in semen analysis testing and a repeat analysis may be required at the time of your visit. It is advantageous to abstain from intercourse for 2-3 days prior to your visit in case a repeat analysis is required. If you prefer to bring a semen analysis back to our laboratory, instructions will be given to you at the time of your visit.
Hormone Testing
Hormone testing includes evaluation of pituitary and testicular function. Hormones produced by the pituitary gland and testicle can impact sperm production and development. This testing involves a blood draw and may include evaluation of follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone and prolactin.
Further Testing
These tests are only ordered when indicated by the history, physical examination, or findings on semen analysis or hormone testing. While some of the more commonly utilized tests are listed below, additional tests exist which your physician will discuss with you if indicated at the time of your visit.
Genetic Testing
- Karyotype.
- Also called a chromosomal analysis, this is a blood test indicated in men with low sperm counts (less than 5 million/mL) or no sperm present in the ejaculate.
- Y-Chromosome Analysis.
- Some men with infertility demonstrate small gene deletions on the Y-chromosome. These “microdeletions” can affect fertility and may be passed on to sons of affected patients. This blood test, as with a karyotype, is indicated in men with low sperm counts (less than 5 million/mL) or no sperm present in the ejaculate.
Imaging
- Transrectal ultrasound.
- Transrectal ultrasound or “TRUS” permits imaging of the prostate, seminal vesicles and ejaculatory duct and is used when ejaculatory duct obstruction is suspected.
- Scrotal Ultrasound.
- Scrotal ultrasound provides detailed imaging of the testicles to assess for size, masses, and consistency. It similarly may be used as an adjunct to the physical exam to confirm the presence of a clinically suspicious varicocele.
Specialized Semen Testing
These tests are utilized to detect abnormalities which are not captured with a routine semen analysis. If indicated, your physician will discuss these tests further with you at the time of your visit.
- Sperm DNA fragmentation.
- DNA fragmentation is primarily a test of sperm quality and is used to assess the stability of DNA packaging within sperm. This test can detect causes of infertility not picked up on a standard semen analysis. Some causes of elevated DNA fragmentation may include smoking, varicocele, and environmental exposures.
- White blood cell assay.
- A high number of white blood cells in the semen may be indicative of an infection, inflammation or anti-sperm antibodies.
- Reactive Oxygen Species.
- Reactive oxygen species or “ROS” are metabolites present in the semen that can be harmful to developing sperm. These can originate from a high number of white blood cells. Elevated levels are a potential contributor to infertility.
- Seminal fructose measurement.
- Fructose is a normal component of the semen. Its absence can suggest that the seminal vesicles may be absent or obstructed.
- Post-ejaculatory urinalysis.
- A post-ejaculatory urinalysis is generally indicated in patients in whom retrograde ejaculation (passage of the semen from the urethra into the bladder) is suspected.
- FISH (Fluorescent in-site hybridization) testing.
- This test uses fluorescent probes to evaluate specific chromosomes. It can identify abnormalities within sperm which can impair fertilization or result in recurrent miscarriage.
- Post-Coital test.
- This test evaluates whether your sperm is compatible with the mucus in your partner’s cervix.
- Viability testing.
- Various tests or stains may be used to assess whether non-moving sperm are alive or dead.
