diaTribe: April 8, 2025 – Lifestyle interventions for managing type 2 diabetes often revolve around weight loss, especially with the rise of GLP-1 medications like Ozempic. While losing weight can improve diabetes management and overall health, making it the main goal can feel overwhelming and lead to changes that are difficult to keep up in the long term without medicine.
Enter glycemic excursion minimization (GEM), a lifestyle intervention that shifts the focus from weight loss to optimizing blood sugar after meals. GEM is a sustainable and effective option for adults with type 2 diabetes not taking insulin.
Key article takeaways:
- Glycemic excursion minimization, or GEM, is a sustainable lifestyle intervention for people with type 2 diabetes that focuses on reducing blood sugar fluctuations after meals rather than weight loss.
- GEM significantly improves A1C levels, reduces diabetes distress, and even leads to diabetes remission in some participants.
- Combining GEM with a continuous glucose monitor improves blood sugar management by providing immediate feedback on the effects of food and activity choices.
How does it work?
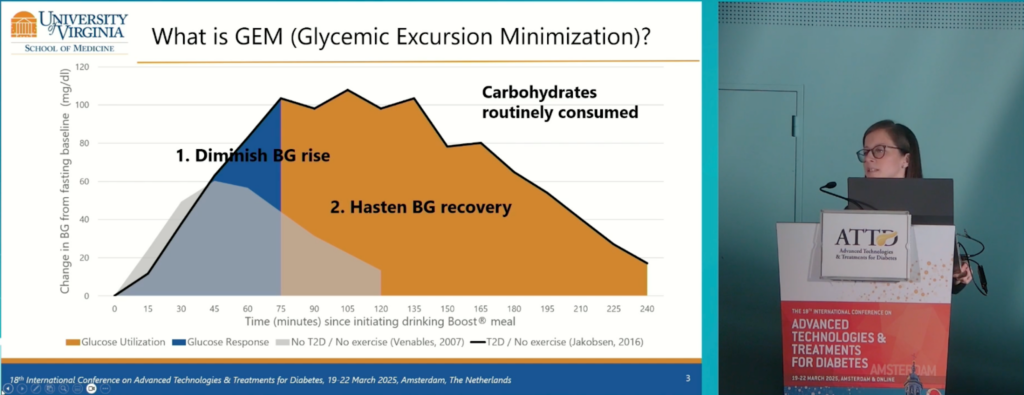
After eating a meal and consuming carbs, blood sugar levels spike and then gradually fall as glucose is absorbed by muscles, fat, and other tissues in a process called blood glucose (BG) recovery.
In people with diabetes, this initial spike is higher and the recovery takes longer because the body’s ability to efficiently process glucose is impaired, leading to prolonged levels of high blood sugar.
Fluctuations in blood glucose levels, particularly after meals, are known as “glycemic excursions,” and GEM aims to minimize these fluctuations. With GEM, the goal is to lower the initial blood glucose rise by choosing lower-carbohydrate foods, and to speed up the recovery period by increasing physical activity after meals, explained Chiara Fabris, Assistant Professor at the University of Virginia, during the 2025 Advanced Technologies and Treatments for Diabetes (ATTD) conference.
Dr. Chiara Fabris presenting at ATTD.
“This can be achieved if we combine the GEM intervention with the use of a continuous glucose monitor (CGM), because the CGM provides immediate feedback on the effect of food and activity choices on glycemic control,” she said.
Fabris described GEM as an empowerment program that educates individuals with type 2 diabetes to make more informed food and physical activity choices, with the support of a CGM.
The intervention lasts about 1.5 months, and includes a guide with exercises and homework, personalized texts reminding users about food and activity choices, and prompts to complete daily diaries. It is split into the following four units:
- Unit 1 (4 days) educates GEM users about the effects of their routine food and activity choices on their blood sugar response with the assistance of a CGM.
- Unit 2 (2 weeks) works on reducing the initial blood sugar spike after meals by limiting and/or replacing foods with a high carb content.
- Unit 3 (2 weeks) focuses on increasing mild and moderate physical activity, especially after eating, to speed up the blood sugar recovery period.
- Unit 4 (1 week) helps to manage relapses by continuing to educate and motivate users on optimizing their food and exercise choices.
Experts have identified specific high-carb (or high “glycemic load”) foods that can be reduced or replaced with options that are less likely to spike blood sugar. They also recommend the mantra, “sit less, step more” to encourage blood sugar uptake after meals, helping to prevent prolonged high blood sugar levels.
What does the research say?
GEM proved to be superior in a study comparing the long-term effects of GEM and traditional weight loss methods in people with type 2 diabetes. While both interventions reduced body mass index, GEM also improved A1C, cholesterol levels, and enhanced diabetes knowledge and empowerment.
Another study found that individuals with type 2 diabetes who used the GEM intervention saw an average A1C reduction of 1.8%, with two-thirds achieving diabetes remission (A1C less than 6.5%). Participants also reported improvements in diabetes distress, diabetes empowerment and depressive symptoms. They also felt that use of the CGM was the most significant single element of the intervention. The researcher who conducted the study says that his own type 2 diabetes has been in remission for 15 years using the GEM approach.
A clinical trial has also shown that participants who used CGM with the GEM intervention had reductions in carbohydrate consumption and the need for diabetes medication, with significant improvements in A1C, diabetes knowledge, and quality of life.
A clinical trial is currently recruiting in Colorado and Virginia to see if individuals with recently-diagnosed type 2 diabetes are able to experience the same benefits with GEM.
The bottom line
GEM is an empowerment program designed to educate people with diabetes on how carbohydrates and physical activity affect post-meal blood sugar levels. By enabling individuals to make informed choices without the restrictions of traditional weight loss programs, GEM offers an effective and sustainable treatment option for people with type 2 diabetes not taking insulin.
