6/20/2025
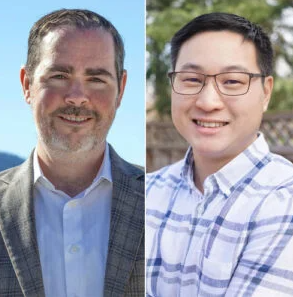
Patrick Finan, PhD, and Philip Chow, PhD, Earn $4 Million to Study an Adaptive Intervention to Manage Low Back Pain - Research - Medicine in Motion News Patrick Finan, PhD,…
Dr. Kim Mathiasen discusses Denmark’s first iCBT services for adults with depression and anxiety
5/9/2025
Dr. Kim Mathiasen, Associate Professor, Aarhus University presented in our CBHT Speaker Series on May 9,2024. Kim Mathiasen, PhD is a licensed clinical psychologist and associate professor at Aarhus University and…
Q&A: What’s Keeping You Up at Night?
3/20/2025
Q&A: What’s Keeping You Up at Night? Nearly a third of adults worldwide have insomnia symptoms, according to the Cleveland Clinic. Struggling to sleep after the time change? You’re not…
Dr. Kara Wiseman featured in Women’s Health: The Lies We’ve Been Told About Alcohol
2/4/2025
The Lies We’ve Been Told About Alcohol The Lies We've Been Told About Alcohol Why experts are now revealing the shocking truth behind alcohol’s “health halo.” By Haley WeissUpdated: Jan 03,…
2/3/2025
Mathematical tools that help social scientists understand the factors that influence how human behavior changes over time are effective at accommodating a small number of variables; however, a recent graduate…
Dr. Steve Ondersma discusses designing sophisticated and interactive digital interventions
2/3/2025
Dr. Steve Ondersma is the C.S. Mott Endowed Professor of Public Health in the Charles Stewart Mott Department of Public Health at Michigan State University, and Director of the e-Health…
1/3/2025
Friday, January 10, 2025 from 9-10am EST Dr. Alexandra Psihogios. Dr. Psihogios is an Assistant Professor in the Department of Medical Social Sciences at Northwestern University in the Feinberg School…
Winner of 2024 CGS/ProQuest Distinguished Dissertation Award: Katharine Daniel
12/6/2024
Winners of 2024 CGS/ProQuest Distinguished Dissertation Awards Announced - CGS Press Release Winners of 2024 CGS/ProQuest Distinguished Dissertation Awards Announced Kelley KarnesIssued: 12-05-24 CGS Contact: Kelley Karnes 602-791-8278 / kkarnes@cgs.nche.edu PDF…
CBS19 Online Insomnia Treatment Can Help Caregivers
9/26/2024
cbs19news.com September 26, 2024 by daf4a@virginia.edu Kelly M. Shaffer, PhD Providing care for a family member with a disabling illness can be a demanding job that leaves many people unable to…
Kelly Shaffer, PhD, and Chongzhi Zang, PhD, Join Cancer Center Leadership
8/8/2024
Kelly Shaffer, PhD, Chongzhi Zang, PhD Kelly Shaffer, PhD, Associate Professor of Psychiatry and Neurobehavioral Sciences, and Chongzhi Zang, PhD, Associate Professor of Genome Sciences, have joined UVA Cancer…