How to Get Involved in Clinical Research
Announcements | About | Research & QI Workflow | Research Forms | How to Get Involved | Contacts

Bhiken I. Naik MBBCh, MSCR
Vice Chair of Clinical Research
Welcome to Clinical Research in the Department of Anesthesiology at the University of Virginia led by the Vice Chair Dr. Bhiken Naik, MBBCh, MSCR. Our work is a collaboration amongst physicians, clinical research coordinators, statisticians, bioinformaticist, and data scientists. Our Clinical research spans both prospective clinical studies and retrospective, observational research.
We work across multiple disciplines and specialties to improve patient safety and identify quality improvement opportunities. We create and define objective metrics to evaluate physician performance and provide opportunities for cost effective and reproducible research.
Furthermore, the Division provides data support to administrative systems within the department and the institution. This includes a generation of reports on clinical practice and outcomes, dashboard maintenance at the departmental and institutional levels, and evaluation and benchmarking of educational activities (e.g. case listings for residents) and clinical workload (e.g. call distribution).
Announcements
About
-
Lauren K. Dunn, MD, PhD
Neuroanesthesia
-
Nabil Elkassabany, MD, MSCE, MBA
Adult Multi-Specialty, Regional
-
Katherine T. Forkin, MD
Liver Transplant
-
Amanda M. Kleiman, MD
Cardiothoracic, Liver Transplant, Obstetrical
-
Lynn R. Kohan, MD
Pain Management
-
Michael Mazzeffi, MD, MPH, MSc, FASA
Critical Care, Cardiothoracic
-
Bhiken I. Naik, MBBCh, MSCR
Critical Care,
Neuroanesthesia
-
Brian Reon, MD, PhD
Neuroanesthesia
-
Robert H. Thiele, MD
Critical Care, Cardiothoracic
-
Mohamed Tiouririne, MD
Critical Care,
Obstetrics
-
Zhiyi Zuo, MD, PhD
Neuroanesthesia
-
Jennifer Phillips RN, CCRC
Clinical Research Manager
JVP8A@uvahealth.org
-
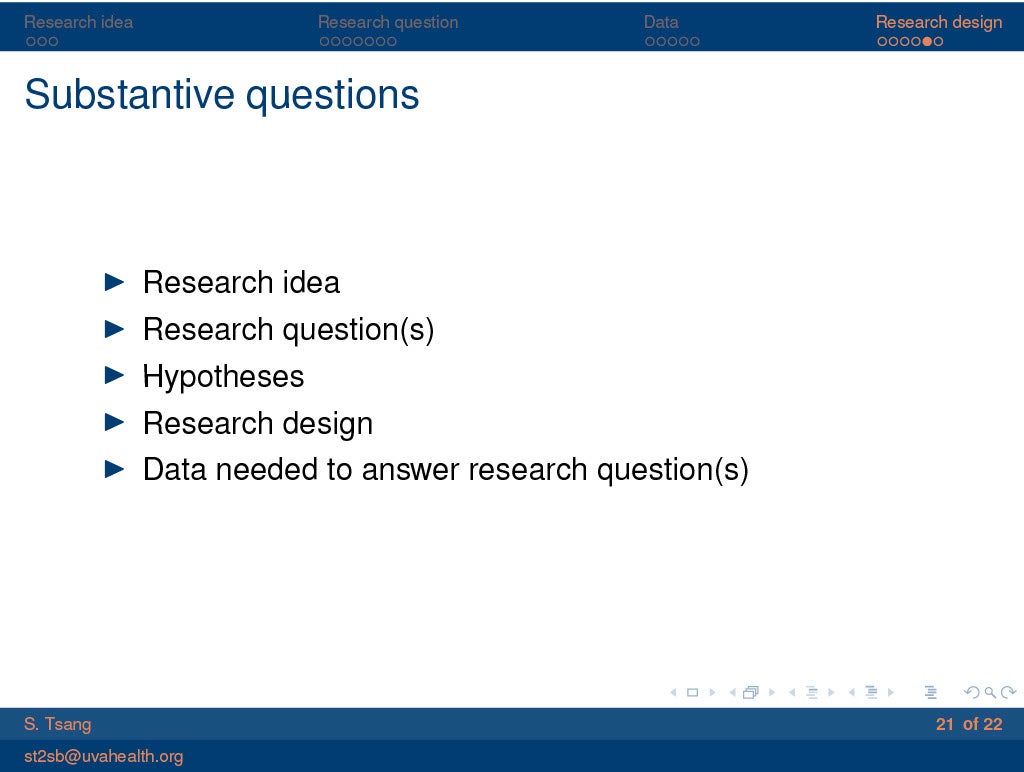
Siny Tsang, PhD
Biostatistician
ST2SB@uvahealth.org
-
Amir Abdel Malek, MS
Data Scientist
AKA5Z@uvahealth.org
-
Ryan Folks, MS
Data Scientist and Machine Learning Engineer
VCZ2AJ@uvahealth.org
-
Emily Chuang, MA
Executive Assistant of Research
QGZ2TK@uvahealth.org
-
Angela Piñeros
CRC4
-
Lucas Fernandez
CRC4
-
Avani Jain
CRC2
-
Ruch Poudyal
CRC2
-
Lexi Moruza
CRC2
-
Meghana Illendula
CRC2
-
Sierra Clark
CRC2
-
Shayan Zakir
CRC2
-
Emily Degen
CRC1
-
Hailey Russo
CRC1
Clinical Research is Actively Supported by the Following Grants:
“Bundle of Love: The effect of self-CARE (Compassion Appreciation Rest and Exercise) on anesthesiology resident wellness” GR014108 GF11096-167460-101, 7/1/2021-6/30/2023
PI: Lauren K Dunn
Non Profit: Foundation for Anesthesia Education and Research
“Smartphone Artificial” GR100450, 9/1/2022-7/31/2023
PI: Bhiken Ishwarlal Naik
Non Profit: Meridian Institute
“Evaluation of the Clinical Performance of the Quantra® System with the QStat® Cartridge in Trauma and Liver Transplantation” GR015881 GI15650-165551-101, 8/27/2020-8/26/2023
PI: Katherine Trumbull Forkin
Industry: HemoSonics, LLC
“An Instrument to Assess the Functional Impact of Chronic Pain Phase II” GR016240 GI16039-169651-101, 10/1/2021-8/31/2023
PI: Lynn R Kohan
Industry: Barron Associates, Inc.
“Discrete Wavelength Frequency Domain Near Infrared Spectroscopy for Non-Invasive Measurement of Cytochrome Oxidation State” GR013755 GB11038-168494-101, 9/21/2021-9/20/2024
PI: Robert Thiele
Federal Government: U.S. NIH Institute of Biomedical Imaging & Bioengineering
“Gut microbiome R21” GR101212, 2/1/2023-1/31/2025
PI: Zhiyi Zuo
Federal Government: U.S. NIH Institute on Aging
“Sedana INSPiRE-ICU1” GR100353, 8/15/2022-8/14/2027
PI: Danny J Theodore
Foreign Industry: Sedana Medical AB
University of Virginia Faculty Select Publications List
January 2025 – May 2025
1. New Kids on the Block: Development and Assessment of a Multispecialty Fascia Iliaca Block Protocol and Training Program for Geriatric Hip Fracture in the Emergency Department.
Kramer JA, Shepherd C, Hess-Homeier D, Ochroch J, Mehta S, Baraniecki-Zwil G, Shofer FS, Elkassabany N, Hussain S, Panebianco N.
Cureus. 2025 Mar 14;17(3):e80560. doi: 10.7759/cureus.80560. PMID: 40225455; PMCID: PMC11994045.
2. What Came First-The Pathology or the Pain?
D’Souza RS, Kohan L, Nelson AM.
Anesth Analg. 2025 Jan 14. doi: 10.1213/ANE.0000000000007275. Epub ahead of print. PMID: 39808727.
3. Pudendal Neuralgia: A Review of the Current Literature
Conic RRZ, Kaur P, Kohan LR.
Curr Pain Headache Rep. 2025 Jan 28;29(1):38. doi: 10.1007/s11916-024-01354-z. PMID: 39873912.
4. Enhancing Early Career Development in Pain Medicine: the Comprehensive Role of Mentorship
Eshraghi Y, Barad M, Pritzlaff S, Emerick T, Wahezi S, Anitescu M, Kohan L.
Pain Med. 2025 Mar 1;26(3):129-130. doi: 10.1093/pm/pnae128. PMID: 39689028.
5. Editorial Review of Qualitative and Quantitative Characteristics of the Lumbar Multifidus Muscles: Comparison of the Magnetic Resonance Imaging and Musculoskeletal Ultrasound
Kohan L.
Interv Pain Med. 2025 Mar 10;4(1):100555. doi: 10.1016/j.inpm.2025.100555. PMID: 40129772; PMCID: PMC11931377.
6. Notable Concerns in Methodology and Conclusions of the Wang et al. Meta-Analysis in BMJ by the American Academy of Pain Medicine.
Schuster NM, Broachwala M, Ahadian FM, Argoff CE, Cohen SP, Durbhakula S, Gulati A, Hurley RW, Kohan L, McCormick ZL, Wahezi SE, Barreveld AM. Pain Med. 2025 Mar 28:pnaf036. doi: 10.1093/pm/pnaf036. Epub ahead of print. PMID: 40156125.
7. Perioperative Lung Expansion and Pulmonary Outcomes After Abdominal Surgery
Blank RS, Ahn HJ.
Lancet Respir Med. 2025 Feb 24:S2213-2600(25)00053-0. doi: 10.1016/S2213-2600(25)00053-0. Epub ahead of print. PMID: 40020693.
8. Protamine Dosing in Cardiac Surgery: Can One Size Fit All?
Mazzeffi M, Levy JH.
Anesthesiology. 2025 Jan 1;142(1):9-11. doi: 10.1097/ALN.0000000000005237. PMID: 39655986.
9. Platelet P2Y12 Receptor Inhibition and Perioperative Patient Management
Mazzeffi M, Tanaka KA, Gurbel PA, Tantry US, Levy JH.
Anesthesiology. 2025 Jan 1;142(1):202-216. doi: 10.1097/ALN.0000000000005148. PMID: 39392789.
10. Fibrinogen Replacement in Neonatal Cardiac Surgery: Methodological Challenges
Butt AL, Mazzeffi MA, Mishima Y, Tanaka KA.
Anesth Analg. 2025 Feb 4. doi: 10.1213/ANE.0000000000007377. Epub ahead of print. PMID: 39903674.
11. Ideal Timing of Coronary Artery Bypass Grafting After Non-ST-Segment Elevation Myocardial Infarction
Norman AV, Weber MP, El Moheb M, Wisniewski AM, Strobel RJ, Speir A, Mazzeffi M, Manchikalapudi A, Joseph M, Tang D, Singh R, Quader M, Beller JP, Yount K, Teman NR.
Ann Thorac Surg. 2025 Feb 11:S0003-4975(25)00113-4. doi: 10.1016/j.athoracsur.2025.01.024. Epub ahead of print. PMID: 39947308.
12. Optimizing Perioperative Extracorporeal Cardiopulmonary Resuscitation Outcomes: Activate Early and Select Carefully
Mazzeffi M, Zaaqoq A, Teman N.
Anesthesiology. 2025 Mar 1;142(3):440-442. doi: 10.1097/ALN.0000000000005323. Epub 2025 Feb 11. PMID: 39932344.
13. Inspired Oxygen Concentration During the Re-initiation of Two-Lung Ventilation in Thoracic Surgery: A Post Hoc Analysis of Data from the Multicenter Perioperative Outcomes Group
Douville NJ, Mathis M, Smolkin ME, Martin LW, Popescu WM, Blank RS.
Anesth Analg. 2025 Mar 10. doi: 10.1213/ANE.0000000000007479. Epub ahead of print. PMID: 40063506.
14. In Vitro Procoagulant Effects of Gla-domainless Factor Xa in Factor XI-deficient and Factor IX-deficient Plasma
Mishima Y, Okada H, Butt AL, Stewart KE, Mazzeffi MA, Tanaka KA.
Thromb Res. 2025 Mar;247:109286. doi: 10.1016/j.thromres.2025.109286. Epub 2025 Feb 15. PMID: 39970742.
15. Cesarean Delivery Outcomes for Patients with Coronavirus Disease-2019 in the USA
Mazzeffi M, Miller D, Garneau A, Sheeran J, Kleiman A, Mehta SH, Tiouririne M.
J Racial Ethn Health Disparities. 2025 Feb;12(1):128-133. doi: 10.1007/s40615-023-01857-2. Epub 2023 Nov 8. PMID: 37938434.
16. Environmental Sustainability in ICUs: A Report From the Society of Critical Care Medicine Sustainability Task Force
Domico M, Meyer MJ, Blackburn L, Toomey SA, Gooch ME, Nadkarni VM, Huckleberry Y, Draper A, Palmieri TL, Nazer LH, Nader A, Valcin EK, Evans S, Al-Hakim T, Murthy S.
Crit Care Med. 2025 Mar 1;53(3):e632-e644. doi: 10.1097/CCM.0000000000006581. Epub 2025 Feb 21. PMID: 39982135.
17. Building an Inclusive Practice within Regional Anesthesia and Acute Pain Medicine
Muse IO, Sabra J, Umeh UO, Elkassabany N.
Anesthesiol Clin. 2025 March; In Press.
18. In Response
Lele AV, Vail EA, O’Reilly-Shah VN, deGrauw X, Domino KB, Walters AM, Fong CT, Gomez C, Naik BI, Mori M, Schonberger R, Deshpande R, Freundlich RE, Mathis MR, Mhyre J, Souter MJ.
Anesth Analg. 2025 Mar 25. doi: 10.1213/ANE.0000000000007503. Epub ahead of print. PMID: 40131819.
19. Formulation of Quality Improvement Methodology for Risk Mitigation in Congenital Cardiac Catheterization
Yeh MJ, Bjornlund E, Gauvreau K, Ali F, Aslam N, Batlivala SP, Berman D, Bocks ML, Chenault K, Doyle T, Gudausky T, Hainstock M, Holzer R, Ibla J, O’Byrne ML, Quinn BP, Shahanavaz S, Sharma R, Trucco SM, Whiteside W, Bergersen L, Armstrong AK.
Pediatr Cardiol. 2025 Jan 14. doi: 10.1007/s00246-024-03738-9. Epub ahead of print. PMID: 39808318.
20. Requesting a Seat at the Table: Fibrin Stabilizing Factor
Sharma R.
Anesth Analg. 2025 Feb 7. doi: 10.1213/ANE.0000000000007413. Epub ahead of print. PMID: 39918995.
21. First-in-human Experience Performing High-resolution Cortical Mapping Using a Novel Microelectrode Array Containing 1024 Electrodes
Konrad P, Gelman KR, Lawrence J, Bhatia S, Jacqueline D, Sharma R, Ho E, Byun YW, Mermel CH, Rapoport BI.
J Neural Eng. 2025 Mar 7;22(2). doi: 10.1088/1741-2552/adaeed. PMID: 39870041.
22. Resigned but Resilient: Caregiver Perceptions of Role Ambiguity and Quality of Care During Hospital-to-Home Transitions of Older Latinos Living with Dementia
Greyson S, Keita M, Sharma R, Yasar S, Boyd C, Keller S, Gurses A, Samus Q, Arbaje A.
J Aging Health. 2025 Mar;37(3-4_suppl):66S-75S. doi: 10.1177/08982643241309443. Epub 2025 Mar 23. PMID: 40123182.
23. Diffuse Myalgia and Neuropathic Pain After COVID Vaccine
Pressler MP, Yaras R, Kohan LR, Singla P.
Pain Med. 2025 Jan 1;26(1):43-44. doi: 10.1093/pm/pnae096. PMID: 39302691.
24. ‘Pain as regional anaesthesia wears off’ or ‘rebound pain’: what’s in a name?
Singla P, Ye Y, Elkassabany NM, Mariano ER.
Anaesthesia. 2025 Mar 3. doi: 10.1111/anae.16583. Epub ahead of print. PMID: 40032279.
25. The Family Anesthesia Experience (FAX): Implementing a Social Support-Focused Wellness Programme Across Multiple Residency Programmes
Martinelli SM, Tran TN, Canter C, Isaak RS, Afroze F, Mulaikal TA, Ladlie B, Jain A, Willie C, Stahl DL, Blanchard E, Zisblatt L, Hoefnagel AL, Marshall JM, Collins S, Keneally RJ, Martin TW, Chen F.
Clin Teach. 2025 Feb;22(1):e13853. doi: 10.1111/tct.13853. PMID: 39710581.
26. Lung Injury in Myocardial Infarction-associated Cardiogenic Shock Supported by Venoarterial Extracorporeal Membrane Oxygenation: A Scoping Review
Zaaqoq AM, Mazzeffi MA, Vogelsong MA, Roeser M, Cho SM.
BMC Cardiovasc Disord. 2025 Jan 23;25(1):40. doi: 10.1186/s12872-025-04472-7. PMID: 39849351; PMCID: PMC11756158.
27. ECMO for the Pregnant and Peripartum Patient: A Practical Review of Indications, Unique Management Considerations, and an Approach Framework.
Hrymak CS, Labib A, Akkanti B, Antonini MV, Bruggeman B, Griffee MJ, Heinsar S, Jacobs JP, Larzelere M, Naoum E, O’Neil E, Roussos-Ross D, Zaaqoq AM, Peek GJ, Arora RC.
Perfusion. 2025 Feb 23:2676591251321070. doi: 10.1177/02676591251321070. Epub ahead of print. PMID: 39988458.
28. Level of Sedation in Patients With COVID-19 Supported With ECMO: A Comparative Analysis of the Critical Care Consortium International Database
Heinsar S, Labib A, Cespedes M, Riera J, White N, Zaaqoq A, Jacobs JP, Buscher H, Alexander PMA, Ciullo A, Aftab M, Suen JY, Bassi GL, Lorusso R, Fraser JF, Peek G; COVID-19 Critical Care Consortium (COVID Critical).
Perfusion. 2025 Feb 26:2676591251324136. doi: 10.1177/02676591251324136. Epub ahead of print. PMID: 40009712.
29. A Retrospective Cohort Study of the Role of Palliative Care Consultation for Patients on Extracorporeal Membrane Oxygenation
Teeri S, Singh P, Gadodia R, Kapil S, Hockstein M, Balsara K, Zaaqoq AM, Rao A.
J Intensive Care Med. 2025 Mar 23:8850666251327105. doi: 10.1177/08850666251327105. Epub ahead of print. PMID: 40123222.
30. Living Alone Predicts Non-Home Discharge Post Elective Hip Arthroplasty: A Matched-pair Cohort Study
Agnor BK, Knio ZO, Zuo Z.
PLoS One. 2025 Jan 2;20(1):e0316024. doi: 10.1371/journal.pone.0316024. PMID: 39746111; PMCID: PMC11694960.
31. Chronic High Fat Diet-induced Cerebrovascular Remodeling Impairs Recovery Of Blood Flow After Cerebral Ischemia In Mice
Li J, Sun N, Hu S, Zuo Z.
J Cereb Blood Flow Metab. 2025 Jan 17:271678X251313723. doi: 10.1177/0271678X251313723. Epub ahead of print. PMID: 39819094; PMCID: PMC11748376.
32. Carboxyl Terminal Modulator Protein Induces Cell Senescence and Is Upregulated with Aging by Zic2 in Rats
Shan W, Li J, Philpot Z, Zuo Z.
J Cell Physiol. 2025 Jan;240(1):e70007. doi: 10.1002/jcp.70007. PMID: 39888066; PMCID: PMC11780686.
33. Pyrrolidine Dithiocarbamate Ameliorates Sepsis-Associated Encephalopathy by Inhibiting Autophagy and Inflammation in the Brain
Lu Y, Zuo Z.
Neurochem Res. 2025 Feb 27;50(2):106. doi: 10.1007/s11064-025-04355-5. PMID: 40011296; PMCID: PMC11865106.
34. Auditory Fear Memory Retrieval Requires BLA-LS And LS-VMH Circuitries Via Gabaergic and Dopaminergic Neurons
Chen M, Li J, Shan W, Yang J, Zuo Z.
EMBO Rep. 2025 Apr;26(7):1816-1834. doi: 10.1038/s44319-025-00403-x. Epub 2025 Mar 7. PMID: 40055468; PMCID: PMC11977213.
35. Are we ready to apply preconditioning-induced neuroprotection to improve the outcome of patients with brain ischemia?
Ren X, Zuo Z.
Translation Medicine Research, In press.
 Through the Multicenter Perioperative Outcome Group (MPOG) we collaborate with multiple institutions world-wide to aggregate millions of cases and billions of data points, which create unparalleled opportunities for both research and quality improvement.
Through the Multicenter Perioperative Outcome Group (MPOG) we collaborate with multiple institutions world-wide to aggregate millions of cases and billions of data points, which create unparalleled opportunities for both research and quality improvement.
Recent projects performed with the MPOG Group include: understanding intraoperative opioid dosing, postoperative respiratory complications, and extubation rates after intracranial surgery.
Research Workflow
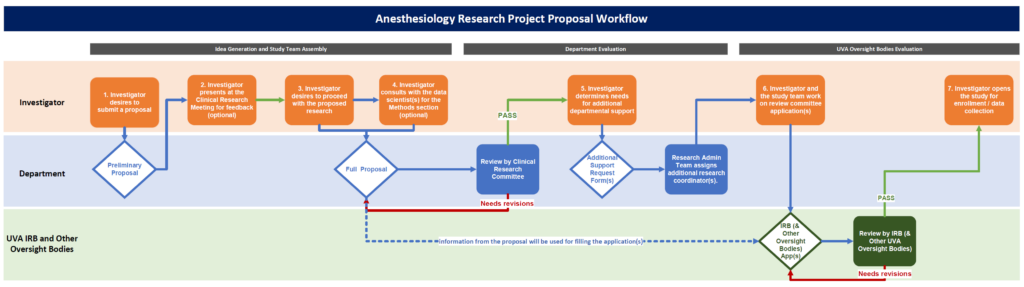
Research Project Proposal Workflow
- Generate a Research Idea
- Find a Faculty Mentor or a Clinical Research Committee member.
- Fill out a Preliminary Proposal Form (at least 1 week prior to the scheduled monthly research meeting if one chooses to present it at the meeting) and receive a copy of your response and your REDCap Survey Queue link in your email.
- Present and Discuss Proposed Research at the Monthly Research Meeting for Feedback (Optional)
- Determine to Proceed with the Proposed Research
- Proceed to fill out a Full Clinical Research Proposal by using the REDCap Survey Queue Link in the preliminary form submission confirmation email.
- Consult with the Data Scientist(s) (Optional)
- If the proposed research is investigator-initiated, please discuss the statistical and power analysis with the data scientist(s) for a well-rounded data analysis plan.
- Determine Needs for Additional Departmental Support
- Fill out a Research Coordinator Request Form and, if applicable, Perioperative Database Request Form in the REDCap Survey Queue.
- If requested, the Clinical Research Admin Team will assign IRB Coordinator, CRC(s), and/or Research Assistants accordingly.
- Work on Review Committee Application(s)
- Discuss with the study team (data scientist, CRCs, RAs, and/or IRB Coordinator) to finalize the study’s protocol for IRB and if applicable other review committees’ application submissions.
- Copy and paste your study’s information from your proposal forms to the application forms when applicable.
- Upon Approvals from the Applicable Review Committee(s), Open the Study for Enrollment/Data Collection
- If requested in the proposal, the departmental data scientist will gather and share the specified perioperative database for the proposed study.
- Regularly check in with the study team regarding enrollment/data collection or analysis progress.
- Please kindly note that each study may require reviews from various boards/agencies depending on what the proposed study entails, and this general workflow instruction is mainly to guide you on creating a proposal for the research admin team to review before further proceeding with obtaining all approvals necessary to begin your proposed study.
For questions, email Dr. Bhiken Naik, Dr. Keita Ikeda, or Emily Chuang, MA.
-
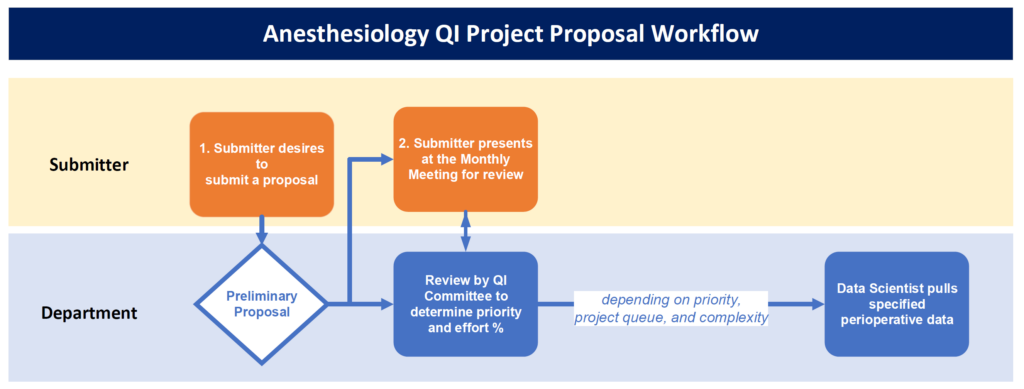
- Generate a quality improvement idea
- Determine if additional research support is needed for the project
- If research support is needed, fill out a Preliminary Proposal Form
- Please do so at least 1 week prior to a Monthly Research Meeting
Please kindly note that depending on the project’s priority, the number of projects in queue, and the complexity of the research support needed, the completion time will differ.
For questions related to research support, please email Dr. Bhiken Naik, Dr. Keita Ikeda, and/or Emily Chuang, MA.
For questions related to QI projects, please email Khaing Phoo and/or Dr. Sunny Chiao.
What is it?
Every month, the department hosts this meeting to talk about research ideas. Studies include prospective, retrospective, observational or multicenter ones. Discussions span from brainstorming ideas to reviewing and finalizing research proposals.
Who is it for?
Anyone interested in research in anesthesiology! We would love to hear your ideas, feedback, and/or questions. Members of the research committee, clinical research coordinators, data scientist, biostatistician and research administrative staff are available to brainstorm ideas with you.
What research ideas will we discuss this time? / What was discussed in a prior meeting?
Please view our agenda and minutes here for the most up-to-date information (link updated 1/23/2024).
What if I have a research idea that I want to discuss?
Great! Please fill out a preliminary proposal down in the Research Forms Section at least 48 hours before the meeting in which you would like to present your proposal.
For more general information on clinical research workflow, please refer to the Research Workflow Section.
When/Where is it?
The meeting will take place once a month on Wednesdays from 12:00pm-1:00pm in OR Classroom A.
If you are not sure how to get there, please email Emily Chuang, M.A. beforehand.
For those who would like to attend virtually, please refer to Zoom link embedded in the department’s Weekly Lecture Schedule email or in the Anesthesiology MASTER Calendar available on Intranet.
Research Forms
- Preliminary Proposal Form for QI or Research (subsequent proposal form links will be emailed upon submission)
- Research Reporting Guidelines Checklist
- Clinical Research Student Assistant Request
How To Get Involved
We welcome inquiries from Medical Students, Residents, and Fellows interested in participating in our department’s research. Please fill out the Interest Form for Clinical Research Involvement, and upon completion, email Emily Chuang, MA.
Contact Us
Emily Chuang, MA
Research Executive Assistant