
By Lisa Farr, M.Ed. Director, Exercise Physiology Core Lab
Interview with Mark De Boer, MD, MSc, MCR, Department of Endocrinology
Parents of pre-teens know that, overnight, it seems like their child is no longer a little kid. Instead, they are a small-sized semi adult with moods, preferences, and a strong desire to exert their independence.
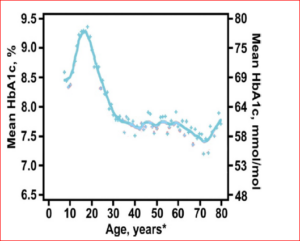
For parents of pre-teens with type1 diabetes, this can be a particularly challenging time. Parents begin to have less control of the child’s schedule, eating habits, and daily behaviors. Of note, the ages of 11- 15 correspond with an incredible rise in hemoglobin A1-C. Hemoglobin A1-C is a blood test that provides a picture about average blood glucose over the preceding 3 months. We know from previous studies that there is an ideal range for HbA1c; while this range will vary a little based on the age and health of the patient, values that are consistently elevated indicate that the diabetes is not under good control. The following graph provides a visual as to what typically happens during adolescence:
Graph Description
Note the large spike in HbA1c during adolescence. Why is this concerning?High HbA1c indicates poor glucose control—i.e, higher blood sugars. Higher blood sugars are associated with many of the complications diabetics face as they get older, such as eye damage, poor circulation and healing, and kidney disease.
For years it was assumed that the large spike in blood sugar seen during the adolescent years was just due to behavioral changes, such as the adolescent assuming a role in diabetes management previously played by parents. But endocrinologists began to suspect there was more to it—might there be physiological reasons as well? It was discovered that the timing of the spike in HbA1c coincided with a spike in levels of hormones that are associated with insulin resistance. Insulin resistance can occur at many different tissues throughout the body, including the liver and muscles. When the cells of the body are more resistant (“less sensitive”) to insulin, blood glucose levels rise.
Dr. Mark De Boer and his colleagues in Endocrinology are studying this issue.
Questions and Answers with Mark De Boer, MD
Question
Why did you want to study diabetes control during adolescence?
Answer
This project addresses what is perhaps the biggest challenge in the clinical care of type 1 diabetics.” “We are examining physiological and psychosocial factors that influence the spike in HbA1c commonly seen in adolescence. We hypothesize that using an artificial pancreas system—an “all in one” diabetes management system that more tightly regulates blood glucose by automatically increasing insulin dose as needed—will in part blunt the rise in HbA1c.
We know that diabetes control—as measured by HbA1c—gets a lot worse during this time frame. We also know that insulin resistance gets worse too. So the thought was—maybe it’s not JUST that these kids are becoming more independent in taking care of their diabetes. Maybe the hormonal changes of adolescence are part of the issue. And if that’s the case—if these normal hormonal changes are partially the culprit—then maybe we, their Physicians, need to be more responsive. Maybe we need to change their care more often during this time. Or maybe an artificial pancreas system, which is a closed loop system that regulates insulin dosing based on current blood glucose level as well as glucose trends, would be the way to go.
Question
So the real life application here is–?
Answer
That we provide better diabetes management during a time when it typically isn’t as good. We know that diabetes management is very important to prevent diabetic complications.
Question
Your study will measure insulin resistance using something called “triple label glucose assessment” and will also measure body composition. Can you tell us a little about each test?
Answer
We’ll bring the kids into the clinical research unit and feed them a meal. We will use a stable isotope tracer (no radiation) to look at insulin and glucose responses at various body tissues in response to the meal. We will also do a yearly Bod Pod body composition test…this allows us to dose the tracer based on how much of their body weight is lean tissue versus fat tissue. It also gives us insight about important shifts in fat and muscle occurring during this period. (the Bod Pod is pictured above)
Study Specifics
Dr. De Boer’s subjects will also be given activity trackers. Exercise and activity are important ways to improve insulin sensitivity and prevent insulin resistance.
Dr. De Boer’s study will enroll type 1 diabetic children who are 11 or 12 years old and follow them for 2 years. The kids in the study will be randomly assigned to either the artificial pancreas system described above, or usual care + CGM. (continuous glucose monitor)
In addition to monitoring HbA1c they will perform a variety of measures at baseline, 12, and 24 months to look specifically at insulin resistance. They will also use surveys and questionnaires to assess for peer relationships, family dynamics, diabetes distress, and other psychosocial markers.
In summary, at the end of this study, Dr. De Boer and his colleagues hope to have better understanding of both the physiological and psychosocial causes for poor diabetes control during adolescence, and whether an artificial pancreas makes a difference.
Their study, funded by the National Institutes of Health, is “Artificial Pancreas-Adolescent Physiology and Psychology Longitudinal Evaluation” (A.P.Apple), HSR 190088.

Mark De Boer and his daughter Arianna.
While catching up with Dr. De Boer about his important new study, we also took a moment to get a little personal too.
Question
What kind of exercise do you do, Dr. De Boer? You look very fit.
Answer
I’ve enjoyed running with my kids…my daughter is now running cross country at William and Mary!… and I also participate in a group called F3, which stands for fitness, fellowship, and faith. We meet a few times each week and do a boot-camp style class that of running, body weight exercises, and all kinds of stuff. Sometimes I even lead the group. It meets bright and early, which is helpful for my schedule.
Question
If you could give health or fitness advice to your younger self what would it be?
Answer
To make time for exercise. Those years of medical school and residency that were so busy—I must have gone years without exercising on a regular basis. You have to carve out time.
