Neuroanesthesia Division
About
Neuroanesthesia as a subspecialty practice in the Department of Anesthesiology at the University of Virginia (UVA) dates back to 1977 when Dr. Robert Bedford joined the department as a faculty member. He became a national figure in neuroanesthesia, publishing clinical findings on intracranial pressure and hemodynamic changes during neurosurgical procedures. The division has other notable alumni, such as Dr. David Stone.
The Neuroanesthesia Division now has 10 faculty members covering the full range of neurosurgery cases and major orthopedic spine cases. These include functional neurosurgery, brain tumor surgery and intracranial aneurysm surgery. There is also a state-of-art facility where intraoperative magnetic resonance imaging (MRI) can be performed. In addition, the University of Virginia hospital is a comprehensive stroke care center. Our faculty covers stroke calls around the o’clock. In total, we perform about 2400 neurosurgical cases each year in the operating rooms
A Message from the Division Chief

Nadia Lunardi, MD, PhD, Neuroanesthesia Division Chief
The Neuroanesthesia Division is very dynamic. Our faculty provide excellent care to patients and also excels in education and research. We have developed a comprehensive educational curriculum for medical students, residents and trained neuroanesthesia fellows.
Faculty academic interests include: education and simulation training, educational research, basic science and translational research, and data science. A unique feature of the division is that three faculty members attend intensive care units, including a neurosurgical intensive care unit. These faculty members provide perspectives on how patients do after surgery and an opportunity to broaden the view of patient care for neurosurgical procedures.
We look forward to collaborative work on education, research and patient care. We also welcome talented people to join us, either as a trainee or as a member of the team.
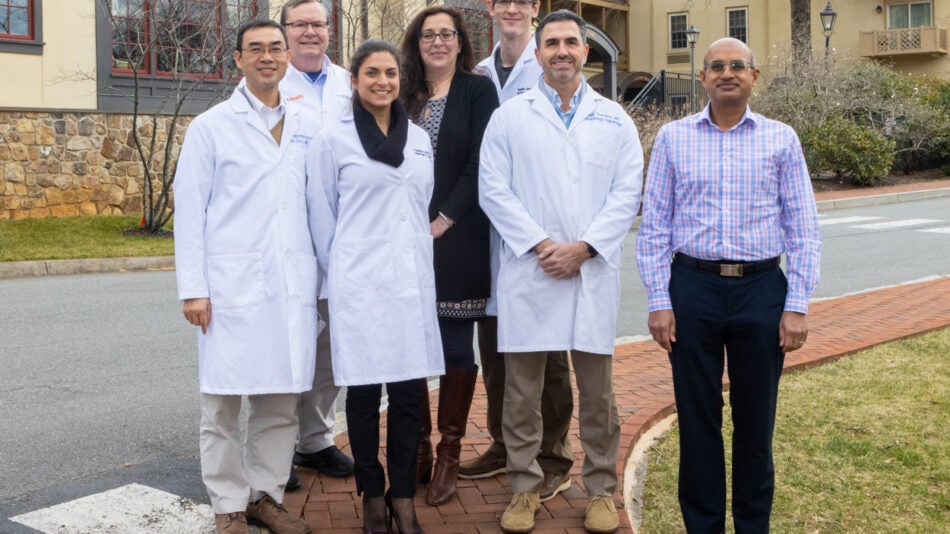
Our Division
-
Nadia Lunardi, MD, PhD
Neuroanesthesia,
Critical Care
-
Vaia T. Abatzis, MD
Neuroanesthesia
-
Lauren K. Dunn, MD, PhD
Neuroanesthesia
-
Tyler J. Johnson, MD
Neuroanesthesia,
Perioperative
-
Emmad Kabil, MD
Neuroanesthesia
-
Bhiken I. Naik, MBBCh, MSCR
Critical Care,
Neuroanesthesia
-
Brian Reon, MD, PhD
Neuroanesthesia
-
Priyanka Singla, MBBS, MD
Pain Management, Neuroanesthesia
-
Danny J. Theodore, MD
Critical Care,
Neuroanesthesia
-
Thaddee Valdelievre, MD
Neuroanesthesia
-
Zhiyi Zuo, MD, PhD
Neuroanesthesia
The Neuroanesthesia Rotation
The Neuroanesthesia Rotation offers a great variety of cases and exposure to complex neurosurgical procedures. These procedures include craniotomy for tumor resection and arteriovenous malformations, endovascular and open treatment of aneurysms, transsphenoidal pituitary surgery, and advanced functional surgeries, such as deep brain stimulator placement, focused ultrasound and epilepsy surgery.
Our renowned spine surgeons perform significantly large spinal fusions (with multiple levels) that require advanced monitoring, and often significant resuscitation. The neuroanesthesia rotation exposes residents to many advanced techniques, including asleep and awake fiberoptic intubation, alternative airway techniques, anesthesia to facilitate neurophysiological monitoring, thromboelastography and ICP monitoring. There are two operating rooms with capability for intraoperative MRI as well as a Comprehensive Stroke Center with a large referral area for interventional thrombectomy procedures.
UVA Neurosurgery and Neurology are consistently ranked in the top fifty in the nation resulting in significant referrals of complex cases. The Neuroanesthesia Division faculty are nationally recognized for our excellence in research and in education.
Society for Neuroscience in Anesthesia and Clinical Care (SNACC)
The Society for Neuroscience in Anesthesia and Critical Care (SNACC) under the Trainee Engagement Committee developed a curriculum resource for residents to utilize during their Neurosurgical Anesthesia rotations.
We divided the core concepts into Basic and Advanced Neuroanesthesia Classrooms with week-by-week guides. The goal is to provide junior and senior anesthesiology residents with focused exposure to PBLDs, articles, and CME questions among other valuable SNACC resources to supplement their learning during a four-week neuroanesthesia rotation.
Johnson T, Gurubhagavatula I. Assessment of Vigilance and Fatigue. Sleep Med Clin. 2023 Sep;18(3):349-359.
Broadhead P, Cook J, Johnson T, Nahass B, Miltner R, McMullan S. Improving Obstructive Sleep Apnea Care in the Postanesthesia Care Unit. J Perianesth Nurs. 2022 Feb;37(1):40-43.
Schnetz MP, Reon BJ, Ibinson JW, Kaynar M, Mahajan A, Vogt KM. Bispectral Index Changes Following Boluses of Commonly Used Intravenous Medications During Volatile Anesthesia Identified From Retrospective Data. Anesth Analg. 2024 Mar 1;138(3):635-644.
Kabil E, Lunardi N, Tennant WG, Esfahani K. Serotonin Syndrome After Prolonged Remifentanil and Propofol Infusion for Craniotomy: A Case Report. A & A Practice 18(6):p e01793, June 2024.
Lele AV, Vail EA, O’Reilly-Shah VN, DeGraw X, Domino KB, Walters AM, Fong CT, Gomez C, Naik BI, Mori M, Schonberger R, Deshpande R, Souter MJ, Mathis MR; MPOG Perioperative Clinical Research Committee. Identifying Variation in Intraoperative Management of Brain-Dead Organ Donors and Opportunities for Improvement: A Multicenter Perioperative Outcomes Group Analysis. Anesth Analg. 2024 Jul 25. Epub ahead of print.
Naik BI, Lele AV, Sharma D, Akkermans A, Vlisides PE, Colquhoun DA, Domino KB, Tsang S, Sun E, Dunn LK; Multicenter Perioperative Outcomes Collaborator Group. Variability in intraoperative opioid and nonopioid utilization during intracranial surgery: A multicenter, retrospective cohort study. J Neurosurg Anesthesiol. 2024 Mar 28. Epub ahead of print.
Esfahani K, Tennant W, Tsang S, Naik BI, Dunn LK. Comparison of oral versus intravenous methadone on postoperative pain and opioid use after adult spinal deformity surgery: A retrospective, non-inferiority analysis. PLoS One. 2023 Jul 21;18(7):e0288988.
Abatzis VT, Park CS, Sumler ML, Littlewood KE. Exploring Fraught Boundaries and Landscapes of Practice. Anesth Analg. 2023 Sep 1;137(3):548-550.
Atluri N, Dulko E, Jedrusiak M, Klos J, Osuru HP, Davis E, Beenhakker M, Kapur J, Zuo Z, Lunardi N. Anatomical substrates of rapid eye movement sleep rebound in a rodent model of post-sevoflurane sleep disruption. Anesthesiology. 2024 Apr 1;140(4):729-741.
Dulko E, Jedrusiak M, Osuru HP, Atluri N, Illendula M, Davis EM, Beenhakker MP, Lunardi N. Sleep fragmentation, electroencephalographic slowing, and circadian disarray in a mouse model for intensive care unit delirium. Anesth Analg. 2023 Jul 1;137(1):209-220.
Vasunilashorn SM, Lunardi N, Newman JC, Crosby G, Acker L, Abel T, Bhatnagar S, Cunningham C, de Cabo R, Dugan L, Hippensteel JA, Ishizawa Y, Lahiri S, Marcantonio ER, Xie Z, Inouye SK, Terrando N, Eckenhoff RG; NIDUS Delirium Network. Preclinical and translational models for delirium: Recommendations for future research from the NIDUS delirium network. Alzheimers Dement. 2023 May;19(5):2150-2174.
Zeng X, Li J, Shan W, Lai Z, Zuo Z. Gut microbiota of old mice worsens neurological outcome after brain ischemia via increased valeric acid and IL-17 in the blood. Microbiome. 2023 Sep 12;11(1):204.
Huang X, Guo M, Zhang Y, Xie J, Huang R, Zuo Z, Saw PE, Cao M. Microglial IL-1RA ameliorates brain injury after ischemic stroke by inhibiting astrocytic CXCL1-mediated neutrophil recruitment and microvessel occlusion. Glia. 2023 Jul;71(7):1607-1625.
Knio ZO, Clancy PW 3rd, Zuo Z. Effect of spinal versus general anesthesia on thirty-day outcomes following total hip arthoplasty: A matched-pair cohort analysis. J Clin Anesth. 2023 Aug; 87:111083.
Education and Training
Neuroanesthesia is a formal rotation for our residents in the department. In addition to patient care related teaching, residents receive education in the simulation center during the clinical rotation. An eight week Neuroanesthesia teaching block with didactic and hand-on teaching workshops runs every two years.
Medical students often rotate with the department and may be assigned with residents to neuroanesthesia cases.
Neuroanesthesia Fellowship
The yearlong Neuroanesthesia fellowship is offered to trainees after successful graduation from an ACGME anesthesia residency. Physicians are hired as Clinical Instructors for this 12 month period. They function as an attending anesthesiologist for 6-10 days per month in the ORs and spend the remainder of days advancing their skills and medical knowledge as a neuro fellow. Research time can be incorporated into this fellowship.
This educational experience requires an understanding of CNS physiology, pathophysiology of neurosurgical disorders, and of the procedures and specific anesthetic techniques, including managing cases requiring neuromonitoring. Fellows will be taught these concepts and their practical applications.
Fellows will frequently be involved in administration of anesthesia for neurosurgical procedures and exposed to emergent neurosurgery and neurotrauma.
Interested applicants should contact Dr. Nadia Lunardi.