By Lisa Farr, M.Ed. Director, Exercise Physiology Core Lab
Interview with: Antonio Abbate, MD, PhD Ruth C. Heede Professor of Cardiology, UVA Cardiovascular Division

We’ve come a long way in how we treat people who are having a heart attack. Even for a “STEMI,” a particularly severe form of a heart attack, prompt treatment with reperfusion and our best medications has decreased acute mortality rates to under 10%.
But while fewer patients die early during the course, those who survive are at significantly higher risk of developing heart failure down the road. Up to 25-30% of STEMI patients develop heart failure at 1-2 years. This is despite our best therapies to preserve heart tissue, prevent abnormal remodeling in the heart, and maintain the heart’s pumping ability. With the burden of heart failure this high, there must be other mechanisms at play.
It has been increasingly recognized that inflammation is a key player in the development of heart failure after a heart attack. Interleukin-1 (IL-1) is an important inflammatory cytokine involved in this process. We know that patients with higher levels of this inflammatory cytokine after a heart attack are more likely to develop heart failure, and are more likely to benefit from anti-inflammatory therapies.
Individuals who go on to develop heart failure after a heart attack are less able to be physically active. They may experience symptoms with exercise, activities of daily living, or, if severe enough, even at rest. Typical symptoms include breathlessness and fatigue. Patients with heart failure report feeling limited during daily life—they are not able to comfortably do the things they want to do. If they have a cardiopulmonary exercise test, their cardiorespiratory fitness is low. Cardiorespiratory fitness is an important predictor of prognosis, as well as quality of life.
Therefore, it is clinically important to prevent this negative cascade of events by developing new therapies which prevent the heart attack patient from developing heart failure. The drug Anakinra, which blocks the inflammatory cytokine IL-1, holds promise in this regard.
Previous studies in animals and humans have indicated that Anakinra significantly blunts the acute inflammatory response seen with a STEMI. When compared to placebo, patients treated with Anakinra have lower rates of new-onset heart failure, and are less likely to be hospitalized for heart failure. The below graphs demonstrate the findings from Dr. Abbate’s previous work in this area.
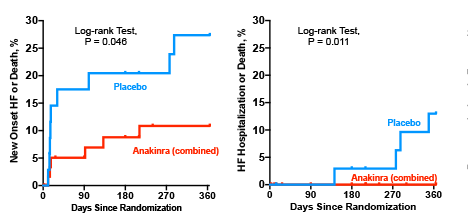
Effects of anakinra of the heart failure events in the VCUART3 study. Anakinra-treated patients had a significantly lower incidence of heart failure related clinical events than placebo. J AM Heart Assoc 2020
Dr. Abbate recently joined the faculty at UVA. His new study will enroll patients at his previous institution (VCU) as well as UVA. The purpose of his new study is to examine the effects of IL-1 blockade with Anakinra on cardiorespiratory fitness, cardiac function, quality of life, inflammatory markers, and incidence of heart failure 6 weeks and one year after a STEMI. Patients admitted for STEMI who meet eligibility and are interested in participating will be randomized to either placebo or 14 days of Anakinra.
Questions and Answers with Dr. Abbate
Question
Why did you want to study this issue?
Answer
I first became interested in this topic as a medical student doing a cardiology rotation. I was doing pre-clinical work studying events in the heart after a heart attack and was fascinated by the overwhelming inflammatory response that occurs immediately, ramps up over the next few days, and then ramps down over the next 2 or 3 weeks. This is when my interest in anti-inflammatory agents to prevent cardiac dysfunction really developed.
Question
So what is the real-life application of your study? How might this improve clinical care?
Answer
The hope, quite simply, is that patients receiving Anakinra will do better and feel better and be less likely to go on to develop heart failure at 6 weeks as well as a year later. We think tempering the acute inflammation seen after a STEMI will be heart-protective—even when patients are already receiving all the currently available recommended therapies. If this turns out to be the case, it gives us one more tool to prevent heart failure and the reduction in fitness and quality of life too commonly experienced after a STEMI.
Question
Can you describe the study?
Answer
If a patient presents to UVA (or VCU) with a STEMI, our team will be alerted. If the care team thinks the patient is eligible for the study, we would come talk to the patient in the CCU—after he/she has received a stent in the artery that caused the heart attack. If the patient is interested in participating, he/she will be randomized to a placebo or Anakinra. A number of tests will occur before the patient leaves the hospital, including labs, and a cardiac MRI. The patient will continue the placebo or Anakinra for the next 14 days. Our team will assess the patient for safety and follow up regularly. Roughly 6 weeks after the heat attack, I will see the patient in clinic, and we’ll do a stress echo in the Exercise Physiology Core Lab. For the stress echo, after we obtain resting echo images, the patient will exercise on a treadmill, and will wear an EKG and a metabolic mask. The patient will push to max and then we will immediately repeat the echo images. Wearing the metabolic mask allows us to measure the patient’s cardiorespiratory fitness and compare this to norms. We think those receiving Anakinra will have higher values—not be as impaired—as those who received placebo. We’ll also do a questionnaire that helps capture how the patient is doing and feeling in life—symptoms, limitations, etc. Six months later the patient will return for a cardiac MRI and then 6 months after that another stress echo. We plan to follow them each year thereafter and our hope is that this treatment given for the first 14 days after a heart attack will be beneficial and prevent heart failure.
The study is UVA HSR 220072 and is entitled Virginia Anakinra Response Trial 4 (Virginia-ART4)
For more information about this project, contact Antonio Abbate at antonio.abbate@virginia.edu
While catching up with Dr. Abbate about his important new study, we took the time to get a little personal too.
Question
Dr. Abbate, you clearly believe in the power of exercise and being fit. What kinds of exercise have you done in your life? What do you do now?
Answer
Exercise is absolutely critical to health—as important as any medication.
Full disclosure—I am not an athlete and never was, but I walk, hike, play pickle ball, and ski. I used to play soccer…but when I grew up in Italy you were encouraged to quit sports if you were a “serious student.” There was this feeling that you couldn’t do both. This is absolutely the wrong approach!
Question
Do you have any advice to others about exercise?
Answer
It can be hard to make time, I know. I have a hard time too. I try to tell my patients this….it’s a struggle most of us have. Talking to them about exercise is always a good reminder for me to keep at it even when I feel too busy.
I think you also have to find activities you enjoy. My daughter Geri plays soccer and field hockey and it has been fun to watch her games and be involved with coaching. Sometimes playing group sports or exercising with others is more motivating to people, makes the time go by, or makes them want to do it. My wife Vera and I like to play pickle ball and go for walks and hike together.

