Critical Care Division
About
The University of Virginia’s Critical Care Division is one of our largest Anesthesiology Divisions. This reflects the growing importance of critical care and perioperative medicine as part of the specialty of anesthesiology, as well as the increased need for intensivists as our population ages and case complexity increases. Our Division has fourteen faculty members and is led by our Division Chief, Robert H. Thiele, M.D.
At UVA, coverage in our three intensive care units (ICUs) are provided by our critical care anesthesiologists. Our three ICUs consist of: Cardiovascular and Thoracic CT-ICU, Neurological (stroke and neurosurgery) NN-ICU, and Surgical/Trauma ST-ICU. All of our neurointensivists are board certified. Some of our intensivists also work as overnight “Rescue” physicians, and during the COVID-19 pandemic we integrated into the broader UVA ICU pool to provide coverage for the special pathogens unit.
A Message from the Division Chief
Robert Thiele, M.D., Critical Care Anesthesia Division Chief
What makes me most proud of the Critical Care Division are the people – despite being the largest division in the Department, we function largely like a family. Our ICU team is professional, well-trained, and collegial – an absolute joy to work with. We also have a variety of individual interests and strengths (e.g. research, teaching, leadership work) that complement each other nicely and lead to a balanced group.
A major feature of the Critical Care Division is the extensive use of ultrasound and an interest in cardiovascular physiology. I am board certified in advanced perioperative TEE, was one of the original question writers for the NBE Examination of Special Competence in Critical Care Echocardiography (CCEeXAM), and hold a Certificate of Completion (COC) for the ACCP’s Critical Care Ultrasonography course. Four of our faculty are TEE-certified and have undergone additional fellowship training in cardiothoracic anesthesia. In addition to bedside transthoracic (and in some cases transesophageal) echocardiography, many of our faculty are competent at performing chest wall ultrasound, abdominal ultrasound, and examining deep venous structures. Our Cardiovascular & Thoracic CT-ICU is particularly rich in the opportunity to utilize bedside ultrasound.
We have fourteen board-certified, full time faculty intensivists, several of whom have dual subspecialty interests (e.g. cardiac anesthesia, neurocritical care board certification). Our faculty come from a variety of institutions, having completed their fellowships at the University of Virginia, University of Florida, Duke University, Vanderbilt, Johns Hopkins, Medical University of South Carolina, Massachusetts General Hospital, University of Chicago, and the University of Michigan. We are currently hiring intensivists to help us grow in all areas of our mission and always interested in hearing from outstanding candidates, including trainees thinking about where they might take their first faculty position.
Our Division
-
Robert H. Thiele, MD
Critical Care, Cardiothoracic
-
R. Ben Alexander, MD
Critical Care
-
Lliam Brannigan, MBBCH
Critical Care, Liver Transplant, Perioperative Medicine
-
Jonathan M. Curley, MD
Critical Care
-
Paul D. Gallo, MD
Critical Care, Cardiothoracic
-
Erin Hennessey, MD
Critical Care,
Perioperative Medicine
-
Ziyad Knio, MD
Critical Care
-
Jenna L. Leclerc, MD, PhD
Critical Care
-
Ryan Lee, MD
Critical Care
-
Nadia Lunardi, MD, PhD
Neuroanesthesia,
Critical Care
-
Michael Mazzeffi, MD, MPH, MSc, FASA
Critical Care, Cardiothoracic
-
Matthew J. Meyer, MD
Critical Care
-
Bhiken I. Naik, MBBCh, MSCR
Critical Care,
Neuroanesthesia
-
Joshua Roach, MD
Critical Care, Cardiothoracic
-
D. Keegan Stombaugh, MD
Critical Care, Cardiothoracic
-
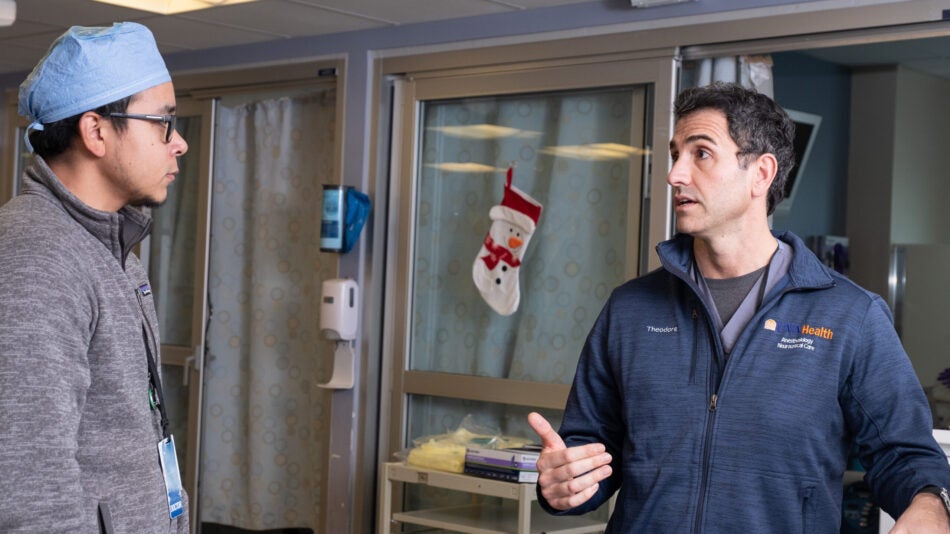
Danny J. Theodore, MD
Critical Care,
Neuroanesthesia
-
Mohamed Tiouririne, MD
Critical Care,
Obstetrics
-
Akram Zaaqoq, MD, MPH
Critical Care

Kierah Barnes, DNP
Kierah Barnes, DNP
Kierah Barnes comes to the University of Virginia from the state of Florida, where she first began her nursing education. In 2023, Kierah completed her Doctor of Nursing Practice at James Madison University. Kierah has been caring for patients as a registered nurse since 2006 when she began her career with Coral Springs Medical Center in Florida, and soon after joined the University of Miami Hospital in the Cardiovascular Intensive Care Unit. Building on her career in intensive care, she went on to work for the Department of Veterans Affairs in the surgical Intensive Care Unit, before finally joining UVA in 2016 as an Acute Care Nurse Practitioner in the Thoracic Cardiovascular ICU. Her focus as a DNP centered around cultural competency training, and racial health disparities during the COVID-19 pandemic. Kierah currently resides in Charlottesville with her husband and 3 children.

Michelle Dawson, MSN, RN, AGACNP-BC, Director of APP Education and Fellowships / Thoracic and Cardiovascular ICU Nurse Practitioner
Michelle Dawson, MSN, RN, AGACNP-BC
Michelle Dawson is an Ohio native, a UK alum, and completed her nursing and masters education at Johns Hopkins and University of Maryland in Baltimore. Upon graduation, she completed a critical care fellowship at the University of Maryland Medical Center / R Adams Cowley Shock Trauma Center where she worked for 7 years. She joined UVA’s Thoracic and Cardiovascular ICU in 2019 and developed UVA’s Advanced Practice Provider (APP) fellowship program. She presently serves as the Director of APP Education and Fellowships and enjoys teaching, particularly on critical care related topics. In her spare time, she enjoys sports, staying active, hiking, and any opportunity to soak up the great outdoors with her husband and three children.

Emily Johnson, PA
Emily Johnson, PA
Emily (Emmy) Johnson is from Richmond, VA. She attended the University of Richmond for undergrad where she played Field Hockey and studied Biology. She worked as a medical/surgical CNA for several years before attending Wake Forest University for PA school. She has been living in the Winston-Salem & Raleigh/Durham area for the past two years and is excited to be back in her home state of Virginia! In her free time, she likes to run, spend time outside, read, and hangout with her husband and her dog, Millie.

Micah Smith, NP
Micah Smith, NP
Hello! I am Micah Smith. I grew up “across the mountain (Afton Mtn)” in Stuarts Draft, Va. I attended UVA for undergrad and then explored several ventures before attending nursing school at PVCC. I began working at UVA’s TCVICU as a PCT in 2014 before beginning as a RN in 2015. I later earned my BSN. In May 2023, I graduated from UVA’s MSN Adult Gerontology Acute Care Nurse Practitioner program. The past year has been a busy one for me but filled with wonderful changes. I am excited to remain in the TCVICU, now as a new Nurse Practitioner. I enjoy our patient population and helping patients and their loved ones through difficult and uncertain times. I love seeing patient progression and the amazing work that people in the TCVICU do.
My wife and I live just outside of Charlottesville. In my free time I enjoy doing anything outdoors. I love spending time on the water, particularly in Virginia’s Northern Neck, and in the mountains. I am passionate about aviation and intrigued by mechanical things. I earned my private pilot’s license in 2008. I am looking forward to doing some flying soon once life settles down a little bit.
I am excited to continue to be a part of the UVA TCVICU team and am eager to begin as a new NP.

Jacqueline Stewart, APP, NP
Jacqueline Stewart, APP, NP
Jacqueline Stewart is originally from Mathews, Virginia. While she is new to this role, she has been working in TCV as an RN for the past several years. She attended UVA for her Nurse Practitioner degree and is excited to follow in the footsteps of several mentors by beginning her NP career at UVA. She loves the patient population at UVA and is humbled by the opportunity to continue learning and growing here. She recently got married and spent the summer training for her second marathon. Outside of work, Jacqueline loves to explore Charlottesville (namely by running and trying local restaurants), cook, read, and spend time with her husband and family.

Sheri Willis, APP, NP
Sheri Willis, APP, NP
Sheri Willis is a TCV RN turned TCV NP! She is a Charlottesville native with a love of coffee, UVA basketball, and tacos. When not at work, you can find her running around with her kids (Teddy, 5 and Sydney, 3), husband (Ryan, old), and dogs (Mac, 15 & Gus, 6 mo.). She enjoys being outdoors as much as possible, listening to music loud enough that it drowns out her singing, staying fit, and reading.
Sheri says she took the long way to get here. She has a BA in History and Classics, but she fell in love with cardiac during nursing school, and has worked in the TCV service line ever since. In May, she graduated from the University of Virginia’s Acute Care NP Program (AGACNP), and she is thrilled to be a part of the TCV ICU APP team!
Our Intensive Care Units
Our Critical Care Division faculty cover the following ICUs:
Cardiovascular and Thoracic CT-ICU
The University of Virginia’s Cardiovascular and Thoracic Intensive Care Unit (CT-ICU) is a 24 bed ICU unit caring for high acuity patients who have undergone various cardiac, thoracic, and vascular procedures. Staffed by a total of 14 attendings of the Department of Anesthesia’s critical care division, and working closely with a team of critical care fellows, residents, and advanced-practice providers, the multidisciplinary team provides care to thousands of ICU patients per year.
The CT-ICU is committed to providing the highest quality training for future leaders, educators, and practitioners of cardiothoracic critical care. We offer a breadth of clinical experience including exposure to:
- Coronary artery bypass surgery
- Minimally invasive valve surgery
- Aortic surgery
- Robotic Thoracic surgery
- Heart and lung transplants
- Ventricular assist devices
- ECMO (Extracorporeal Membrane Oxygenation)
- Pulmonary endarterectomy
- Structural Heart procedures
In the ICU, critical care fellows organize teaching/work rounds, formulate care plans, and facilitate communication between the ICU team and surgical services, consultative services, and family members.
Neurological NN-ICU
Our department shares equal coverage of our Neurology ICU with critical care trained neurologists. All of our neurointensivists are board-certified or in the process of seeking additional subspecialty certification. In the NN-ICU we care for patients who have experienced stroke (ischemic and hemorrhagic), seizure disorders, traumatic brain injury, cerebral aneurysm rupture, major spine surgery, as well as less common but life-threatening neurological disorders.
Surgical ST-ICU
On the Surgical and Trauma ST-ICU, we care for patients from several different surgical specialties including solid organ transplant, general surgery, major orthopedic surgery, plastics, ENT, urology and OBGYN. This creates an interesting mix of patients, clinical issues and management strategies. It presents challenges in communication and care coordination, but we are fortunate to have good professional relationships with our surgical colleagues as well as a culture that encourages professionalism and collegiality.
We have a multidisciplinary attending team that consists of trauma/surgical ST-ICU and anesthesiology intensivists who provide an interesting mixture of perspectives, approaches and teaching. All of our attendings are interested in teaching and supervising.
The resident staff come from surgery, anesthesiology and emergency medicine. They again provide a blend of thought processes and perspectives. We have a very solid and long-term team of NPs that are there for advice and help – and happily provide assistance in a collegial manner. The NPs and residents work very well together, and we encourage mutual support.
Overall, the ST-ICU is an interesting blend of patients, clinical issues, care teams, faculty and staff that provide a good education in a wide range of clinical problems within a supportive, collegial culture.
SPU/MICU
Drs. Theodore and Thiele spent time working in the Special Pathogens Unit (SPU) during the COVID-19 pandemic. Dr. Theodore continues to work in the MICU as a nocturnist, building important bridges between our division and our pulmonary-CCM colleagues.
Two of our intensivists were recently awarded K-08 funding from the NIH. The research interests of our division are broad, and include neurocognitive dysfunction and sleep disturbances in the ICU setting (Nadia Lunardi, M.D., Ph.D.), perturbations in subcellular energetics, the potential role of exercise “preconditioning” in protecting patients from sepsis, advanced hemodynamic monitoring, right ventricular protection (Robert Thiele, MD), and a variety of database work conducted through both STS and MPOG (Naik).
Research Interests
Neurocognitive dysfunction
Sleep disturbances in the ICU setting
Perturbations in subcellular energetics
Exercise “preconditioning”
Advanced hemodynamic monitoring
Right ventricular protection
Database research (MPOG)
Research Funding
Apple: Thiele
Engineering in Medicine: Thiele
NIH (NINDS, K-08): Lunardi
NIH (NIGMS, K-08): Thiele
IARS Mentored Research Award: Lunardi
Society of Cardiovascular Anesthesiologists: Thiele
Ivy Foundation: Thiele
Publications
Thiele RH. Sarosiek BM. Modesitt SC. McMurry T. Tiouririne M. Martin L. Blank RS. Shilling A. Browne J. Bogdonoff D. Bauer T. Hedrick TL. “Development and Impact of an Institutional Enhanced Recovery Program on Opioid Use, Length of Stay, and Hospital Costs within an Academic Medical Center: A Cohort Analysis of 7,774 Patients.” Anesthesia & Analgesia 132: 442-455, 2021 [PMID: 33105279].
Osuru HP, Paila U, Ikeda K, Zuo Z, Thiele RH. “Anesthesia-Sepsis-Associated Alterations in Liver Gene Expression Profiles and Mitochondrial Oxidative Phosphorylation Complexes.” Front Med (Lausanne). 7: 581082, 2020 [PMID: 31307382].
Hedrick TL, Hassinger TE, Myers E, Krebs ED, Chu D, Charles AN, Hoang SC, Friel CM, Thiele RH. “Wearable Technology in the Perioperative Period: Predicting Risk of Postoperative Complications in Patients Undergoing Elective Colorectal Surgery.” Dis Colon Rectum 63: 538, 2020 [PMID: 32015289].
Saugel B. Thiele RH. Hapfelmeier A. Cannesson M. “Technological Assessment and Objective Evaluation of Minimally-Invasive and Non-Invasive Cardiac Output Monitoring Systems.” Anesthesiology 133: 921, 2020 [PMID: 32773696].
Yoon U, Bartoszko J, Bezinover D, Biancofiore G, Forkin KT, Rahman S, Spiro M, Raptis DA, Kang Y; ERAS4OLT.org Working Group. “Intraoperative transfusion management, antifibrinolytic therapy, coagulation monitoring and the impact on short-term outcomes after liver transplantation – A systematic review of the literature and expert panel recommendations.” Clin Transplant. 2022 Mar 6;e14637. doi: 10.1111/ctr.14637. Online ahead of print.
Thiele RH, Ikeda K, Osuru HP, Zuo Z. “Comparison of Broadband and Discrete Wavelength Near Infrared Spectroscopy Algorithms for the Detection of Cytochrome aa3 Reduction.” Anesthesia & Analgesia 129: 1273, 2019 [PMID: 29916864].
Naik BI, Kuck K, Saager L, Kheterpal S, Domino KB, Posner KL, Sinha A, Stuart A, Brummett CM, Durieux ME, Vaughn MT, Pace NL; MPOG EOS Investigator Group. “Practice Patterns and Variability in Intraoperative Opioid Utilization: A Report From the Multicenter Perioperative Outcomes Group.” Anesth Analg. 2021. [PMID: 34291737].
Mayer SA, Frontera JA, Jankowitz B, Kellner CP, Kuppermann N, Naik BI, Nishijima DK, Steiner T, Goldstein JN; CNS Bleeding/Neurosurgery Subgroup of the NHLBI Hemostasis Trials Outcomes Working Group. “Recommended Primary Outcomes for Clinical Trials Evaluating Hemostatic Agents in Patients With Intracranial Hemorrhage: A Consensus Statement.” JAMA Netw Open. 2021, [PMID: 34473266].
Colquhoun DA, Leis AM, Shanks AM, Mathis MR, Naik BI, Durieux ME, Kheterpal S, Pace NL, Popescu WM, Schonberger RB, Kozower BD, Walters DM, Blasberg JD, Chang AC, Aziz MF, Harukuni I, Tieu BH, Blank RS. “A Lower Tidal Volume Regimen during One-lung Ventilation for Lung Resection Surgery Is Not Associated with Reduced Postoperative Pulmonary Complications.” Anesthesiology. 2021, [PMID: 33635945].
Illendula M, Osuru HP, Ferrarese B, Atluri N, Dulko E, Zuo Z, Lunardi N. “Surgery, anesthesia and Intensive Care environment induce delirium-like behaviors and impairment of synaptic function-related gene expression in aged mice.” Front Aging Neurosci 12:542421, 2020 [PMID:33088271].
Hilton EJ, Goff KL, Sreedharan R, Lunardi N, Batakji M, Rosenberger DS. “The flaw of Medicine: addressing racial and gender disparities in Critical Care.” Anesthesiol Clin 38(2):357, 2020 [PMID:32336389].
Lunardi N, Sica R, Atluri N, Salvati KA, Keller C, Beenhakker MP, Goodkin HP, Zuo Z. “Disruption of Rapid Eye Movement sleep homeostasis in adolescent rats after neonatal anesthesia.” Anesthesiology 130(6):981, 2019 [PMID:30946702].
Education is an important focus of our division. We have an ACGME-accredited fellowship led by Fellowship Director Dr. Naik, M.B.B.Ch., and we accept two fellows a year. Anesthesiology and surgery residents rotate regularly through all of our ICUs.
Undergraduate Medical Education
Many of our medical students who are interested in anesthesiology and/or critical care spend a month rotating through our CT-ICU. This ICU is staffed almost exclusively by anesthesiologists, which allows them to get to know our faculty, many of whom write their letters of recommendation for residency positions.
Residency
Our four-year anesthesiology residents spend one month in our Pediatric ICU, ST-ICU, neuro NN-ICU, and CT-ICU. Three year residents (who do an internship elsewhere) spend one month in our ST-ICU, neuro NN-ICU, and CT-ICU. All residents are offered the opportunity to do additional elective time in any of our ICUs during their CA-3 year.
Fellowship in Critical Care
We offer a one year Fellowship in Critical Care Anesthesiology, and can accept up to four fellows per year. Our fellowship is highly flexible and can be tailored to the needs of the individual, with elective opportunities in a variety of consulting services (e.g. nutrition) as well as in clinical research, and in transesophageal echocardiography.
Our fellowship is not limited to anesthesiologists. We have trained board-eligible general surgeons and we welcome the opportunity to train intensivists with a background in emergency medicine.
More About Education
Our fellows serve as instructors for residents, medical students, nurse practitioners, and nursing staff. Fellowship didactics throughout the year include case-based presentations, journal clubs, POCUS and TEE training, participation in simulation sessions, and board review sessions throughout the year.
Residents in the Department of Anesthesia rotate for 1 month in the ICU Division during their CA-1 year and continue to hone their skills in the post-operative management of critically ill patients. Residents gain exposure to a variety of uncommon operating room procedures, including diagnostic and therapeutic bronchoscopies, thoracentesis and chest tube placement, and placement of dialysis catheters. Residents interested in critical care medicine and cardiothoracic anesthesia can also begin their training in transesophageal echocardiography and the requirements for the basic transesophageal echocardiography exam (Basic PTeEXAM).
The CT-ICU also serves a large role in the School of Medicine as a site for the medical student Advanced Clinical Elective (ACE) program. The ACE program includes a 4-week clinical rotation during which time students develop advanced clinical skills as they take on increased responsibilities for the evaluation and management of patients. ACE Students are integrated as members of the healthcare team and focus on the management of multi-system disease. They become skilled in the diagnosis and management of respiratory, cardiovascular, metabolic, and hemodynamic compromise and they develop treatment plans under supervision from an attending. ACE Students receive feedback in preparation for the start of residency training.