Pain Management Division
About
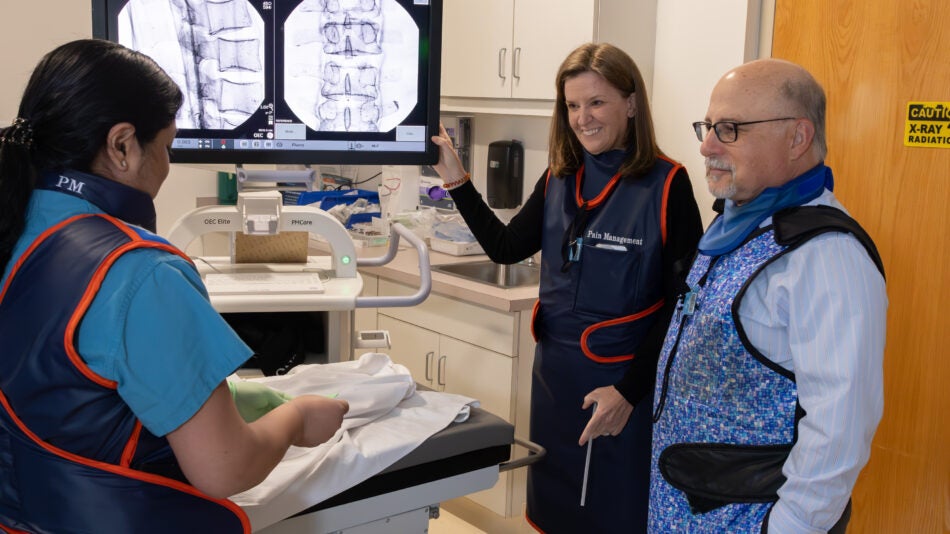
The University of Virginia (UVA) Department of Anesthesiology Pain Management Division offers multidisciplinary care for a wide range of pain conditions. The UVA Pain Management Center has been designated as a Center of Excellence by the American Pain Society. The division provides care for patients with over 10,500 visits per year. Our Division has six board certified pain medicine physicians in addition to pain psychologists and a nurse practitioner and is led by Lynn Kohan M.D., our Pain Management Division Chief. One of our pain physicians, Dr. Robert Goldstein, is also board certified in palliative medicine.
At UVA, the Pain Management Center provides coverage for both outpatient care (clinic visits and interventional management) and inpatient care through the hospital pain service. Major features of the Pain Management Division include extensive expertise in complex pain management, advanced interventional treatments (including neuromodulation and intrathecal drug delivery). Our physicians treat a wide range of pain conditions, including cancer pain, spine related disorders, complex regional pain syndrome, and joint disease.
A Message from the Division Chief

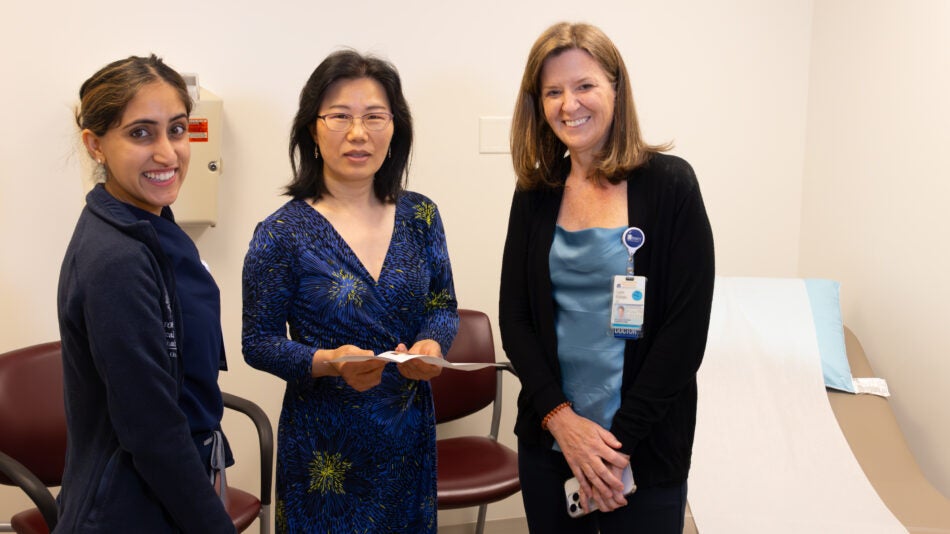
Lynn Kohan, MD, Pain Management Division Chief
We have a very talented group of pain management physicians at UVA with a wide range of interests and skills. Our clinicians are highly regarded for their clinical expertise and commitment to education. Many of our faculty are recognized both on a regional and/or on a national level. The Pain Management Division Faculty also serve on numerous pain medicine committees and editorial boards.
Our goal is to provide comprehensive pain management and provide excellent education to our trainees. Our division members give formal lectures in all aspects of pain medicine, provide hands-on training in simulation (crisis management of pain procedures), as well as care for and educate our patients.
Our Division
-
Lynn R. Kohan, MD
Pain Management
-
Peter E. Amato, MD
Pain Management
-
Dania C. Chastain, PhD
Pain Management
-
Patrick H. Finan, PhD
Pain Management
-
Matthew D. Holland, MD
Pain Management
-
Christina Shin, MD
Pain Management
-
Priyanka Singla, MBBS, MD
Pain Management, Neuroanesthesia
-
Lori A. Urban, PsyD, ABPP
Pain Management
-
Bhavana Yalamuru, MBBS
Pain Management
-
Xiaoying (Amy) Zhu, MD
Pain Management
The Pain Management Division provides care for a wide range of painful conditions. We emphasize a multimodal approach that may utilize medication management, interventional techniques, as well as non-pharmacologic modalities. Patients may be new to pain management, or they may seek additional treatment options from our tertiary care center.
Neuromodulation
Pain management centers offer the latest in a variety of advanced technologies to treat painful conditions including the use of spinal cord stimulation, peripheral nerve stimulation, and intrathecal drug delivery systems.
Cancer Pain
Our clinicians provide the latest advancements in cancer related pain. They often work in collaboration with oncologists and palliative care clinicians to provide comprehensive care.
Our division provides management of a large intrathecal drug delivery population for management of cancer related pain, spasticity, and non-malignant pain.
For patients with complex regional pain syndrome, we provide an unique continuous ketamine infusion program. We are also involved in developing areas for pain treatment including the use of focused ultrasound.
Perioperative Pain
Our Perioperative Pain Clinic offers comprehensive care during the perioperative period. Patients may be referred prior to surgery where they undergo medical, psychologica, and physical conditioning to optimize pain control throughout this time. Patient care is continued during the in-patient admission and up to 90 days postoperatively.
Pain Psychology
The Pain Management Division offers comprehensive treatment in pain psychology, including the use of modalities such as increasing coping mechanisms, relaxation techniques, and biofeedback.
 Our clinicians are involved in research, having been awarded both National Institutes of Health (NIH) and industry funded grants. Research areas include: radiofrequency ablation of joints (knee and sacroiliac), microdosing in intrathecal drug delivery, objective measurements of pain, evaluation of ketamine infusion in the use of chronic pain conditions, and the use of focused ultrasound. Additional research is devoted to education and gender disparities.
Our clinicians are involved in research, having been awarded both National Institutes of Health (NIH) and industry funded grants. Research areas include: radiofrequency ablation of joints (knee and sacroiliac), microdosing in intrathecal drug delivery, objective measurements of pain, evaluation of ketamine infusion in the use of chronic pain conditions, and the use of focused ultrasound. Additional research is devoted to education and gender disparities.
McCormick ZL, Cohen SP, Walega DR, Kohan L. “Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes.” Reg Anesth Pain Med. 2021 Jun;46(6):518-523. doi: 10.1136/rapm-2020-102117. Epub 2021 Jan 22. PMID: 33483425.
Michaud K, Cooper P, Abd-Elsayed A, Kohan L. “Review of Radiofrequency Ablation for Peripheral Nerves.”
Curr Pain Headache Rep. 2021 Oct 7;25(10):63. doi: 10.1007/s11916-021-00981-0.
Kohan L, Potru S, Barreveld AM, Sprintz M, Lane O, Aryal A, Emerick T, Dopp A, Chhay S, Viscusi E. “Buprenorphine management in the perioperative period: educational review and recommendations from a multisociety expert panel.” Reg Anesth Pain Med. 2021 Oct;46(10):840-859. doi: 10.1136/rapm-2021-103007. Epub 2021 Aug 12.
Chen AF, Khalouf F, Zora K, DePalma M, Kohan L, Guirguis M, Beall D, Loudermilk E, Pingree MJ, Badiola I, Lyman J. “Cooled radiofrequency ablation provides extended clinical utility in the management of knee osteoarthritis: 12-month results from a prospective, multi-center, randomized, cross-over trial comparing cooled radiofrequency ablation to a single hyaluronic acid injection.” BMC Musculoskelet Disord. 2020 Jun 9;21(1):363. doi: 10.1186/s12891-020-03380-5. PMID: 32517739.
Chen AF, Khalouf F, Zora K, DePalma M, Kohan L, Guirguis M, Beall D, Loudermilk E, Pingree M, Badiola I, Lyman J. “Cooled Radiofrequency Ablation Compared with a Single Injection of Hyaluronic Acid for Chronic Knee Pain: A Multicenter, Randomized Clinical Trial Demonstrating Greater Efficacy and Equivalent Safety for Cooled Radiofrequency Ablation.” J Bone Joint Surg Am. 2020 Sep 2;102(17):1501-1510. doi: 10.2106/JBJS.19.00935.
Sperry BP, Conger A, Kohan L, Walega DR, Cohen SP, McCormick ZL. “A Proposed Protocol for Safe Radiofrequency Ablation of the Recurrent Fibular Nerve for the Treatment of Chronic Anterior Inferolateral Knee Pain.” Pain Med. 2021 May 21;22(5):1237-1241. doi: 10.1093/pm/pnaa291.
McCormick ZL, Cohen SP, Walega DR, Kohan L. “Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes.” Reg Anesth Pain Med. 2021 Jun;46(6):518-523. doi: 10.1136/rapm-2020-102117. Epub 2021 Jan 22.
Mendelson AM, Kohan L, Okai J, Wanees M, Gonnella JC, Torjman MC, Viscusi ER, Schwenk ES. “Adverse drug effects related to multiday ketamine infusions: multicenter study.” Reg Anesth Pain Med. 2020 Feb 12:rapm-2019-101173. doi: 10.1136/rapm-2019-101173. Online ahead of print.
Kohan L, Moeschler S, Spektor B, Przkora R, Sobey C, Brancolini S, Wahezi S, Anitescu M. “Maintaining High-Quality Multidisciplinary Pain Medicine Fellowship Programs: Part I: Innovations in Pain Fellows’ Education, Research, Applicant Selection Process, Wellness, and ACGME Implementation During the COVID-19 Pandemic.” Pain Med. 2020 Aug 1;21(8):1708-1717. doi:10.1093/pm/pnaa168. PMID: 32632454.
Kohan L, Sobey C, Wahezi S, Brancolini S, Przkora R, Shaparin N, Spektor B, Moeschler S, Anitescu M. “Maintaining High-Quality Multidisciplinary Pain Medicine Fellowship Programs: Part II: Innovations in Clinical Care Workflow, Clinical Supervision, Job Satisfaction, and Postgraduation Mentorship for Pain Fellows During the COVID-19 Pandemic.” Pain Med. 2020 Aug 1;21(8):1718-1728. doi:10.1093/pm/pnaa176. PMID: 32379882.
Yalamuru B, Weisbein J, Pearson ACS, Kandil ES. Ann “Minimally-invasive pain management techniques in palliative care.” Palliat Med. 2021 Aug 16:apm-20-2386. doi: 10.21037/apm-20-2386. Online ahead of print. PMID: 34412500.
Yalamuru B, Dexter F, Silver JK, Moeschler SM, Pearson ACS. “Representation of women as editors in major pain journals.” Reg Anesth Pain Med. 2021 r;46(4):356-357. doi: 10.1136/rapm-2020-101675. Epub 2020 Nov 16.
Zhu X, Bratanow NC. “Physician Perspective and Challenges Ordering/Interpreting Laboratory Tests Related to the Opioid Crisis in America.” Ther. Drug Monit. 2021 Feb 1;43(1):6-13. doi: 10.1097/ FTD.0000000000000840. PMID: 33230042.
Zhu X, Kohan LR, Morris JD, Hamill-Ruth RJ. “Sympathetic blocks for complex regional pain syndrome: a survey of pain physicians.” Reg Anesth Pain Med. 2019 May 3:rapm-2019-100418. doi: 10.1136/rapm-2019-100418. Online ahead of print. PMID: 31055496.
Zhu X, Kohan LR, Goldstein RB. “Substantial Elevation of Liver Enzymes During Ketamine Infusion: A Case Report.” A A Pract. 2020 Jun;14(8):e01239. doi: 10.1213/XAA.0000000000001239. PMID: 32643900; PMCID: PMC7323839.
Please see the UVA Office of Pain Management and Opioid Stewardship (OPMOS) webpage.
Education and Training:
Residency
Our Interns and 3rd year Anesthesia Residents rotate in the Pain Management Center (PMC). Residents participate to provide medical and interventional care to our patients. Residents also rotate on the Hospital Consult Service (CPS).
Multidisciplinary Fellowship in Pain Medicine
The fellow’s year on the Pain Services is spent in the (chronic) Pain Management Center (PMC) and on the In-Hospital Consult Service (CPS). Approximately 70% of the time is spent in the Pain Management Center. This time is divided between the clinic where they see 8-10 patients per day, and perform approximately 15 interventional procedures per day. In addition, fellows also perform interventional procedures at the nearby Monticello Surgery Center that is affiliated with UVA. These procedures encompass a varied assortment of pain management techniques.
The daily clinic schedule is a blend of new patients and revisits. Twenty percent of the time is spent leading the CPS which runs a daily census of 5-10 consult patients. Fellows’ time is also dedicated to the ACGME mandated rotations which include physical medicine and rehabilitation, psychiatry, neurology, and anesthesiology/airway management.
Fellows rotate through the services that are not their primary specialty. Generally, these rotations are one week long. Additionally, fellows gain experience in the operating room, where they perform advanced interventional techniques including neuromodulation, intrathecal drug delivery systems, Osteocool, MILD and kyphoplasty.