Program Features
Fast Facts
- One year, clinical geriatric medicine fellowship
- Class size: 2 fellows per year
- Block rotation schedule designed to provide breadth of sub-specialty experiences critical to geriatric practice (see below)
- Longitudinal experiences designed to provide depth of training in core geriatric principles, in both clinic and residential care facility settings
- No clinical responsibilities on weekends. No in-house call. Fellows are on call by phone for 8 to 11 weeks per year with back-up faculty geriatrician available at all times
- 3 weeks of vacation leave
- 5 days of professional leave for educational activities. Of note, attendance at the AGS annual conference is mandatory and will not count against a trainee’s 5 days.
- PGY4 stipend for academic year 2023-2024 was $69,440 plus $2,500 for education-related expenses. For the 2023-2024 academic year, we also offered an additional $10,000 signing bonus
Clinical Experiences
Block Rotation Schedule
Outpatient Care
- Primary care clinics with geriatric-only populations, attended by board-certified geriatricians. The practice consists of preventative medicine, acute care and coordination of subspecialty care for our longitudinal patients. There are currently several such clinics, as described here. Fellows will be placed in one clinic for a longitudinal primary care experience.

The Colonnades Medical Associates clinic is staffed by two geriatricians and has on-site services for phlebotomy, EKGs and nursing support.
- Memory Disorders clinic is a subspecialty clinic specializing in neurocognitive disorders which is currently a collaborative effort involving Neurology, Neuropsychology and Geriatric Medicine faculty.
- Subspecialty clinics: Neurology, Pain, Endocrine, Wound, among others listed above in the block schedule.
Inpatient Care
- Consultative Geriatric Medicine experience on the Orthopedic-Medicine service
- Consultative Palliative Medicine experience at the University of Virginia Hospital
- Consultative Geriatric Psychiatry experience at the University of Virginia Hospital
- Evaluation and management of geriatric patients at the University of Virginia Encompass Rehabilitation Hospital, alongside Physical Medicine and Rehabilitation faculty attendings
Residential Facility Care
- Skilled nursing facilities with clinical exposure to both long-term care, custodial patients as well as short term, acute rehabilitation patients

Fellows will have a longitudinal skilled nursing facility experience at Westminster Canterbury of the Blue Ridge and will work closely with Dr. Thomas Bradley Murray to provide care.
- Assisted living facilities with clinical exposure to patients with functional and/or cognitive deficits.

Fellows will work in multi-disciplinary teams with nurses, physician assistants and nurse practitioners to care for patients at the Colonnades Assisted Living facility
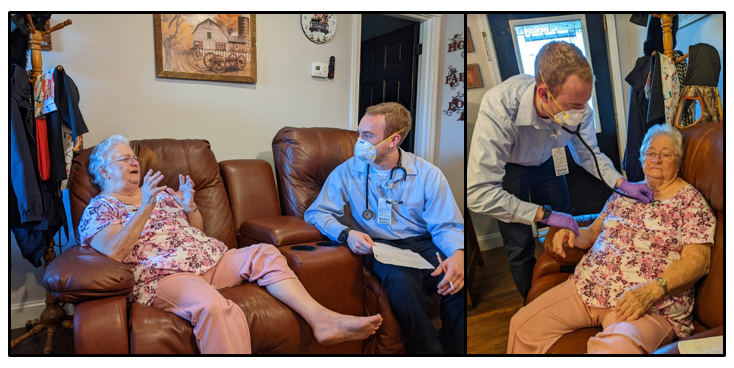
Home-Based Primary Care
- The Virginia at Home Program which cares for its homebound patients with a multi-disciplinary team providing near 100% of their care within the patient’s home. Fellows will have a block rotation with the Virginia at Home Program. For more information, please see: Virginia at Home Program – Population Health.
Didactic Experiences
Journal Club: Occurs once per month. Each fellow presents a current geriatric medicine article to the section.
Core Geriatric Lectures: Designed to cover the breadth of geriatric curricular milestones as outlined by the American Geriatric Society. Lectures are presented by both geriatricians and subspecialists depending on the subject.
Health Systems and Impact on Geriatric Medicine: A mini-series of lectures covering a variety of community geriatric care models, value-based care, and Medicare, among other topics.
Board Review Curriculum: Longitudinal, fellow-driven curriculum where fellows have the opportunity to research and provide short teaching sessions on testable topics once a month. This is capped by a mini-series of lectures provided by geriatric faculty at the end of the year, followed by a practice exam, designed to prepare fellows taking the Geriatric Medicine subspecialty board exam.
Career Advancement
Medical Directorship: A mini-series of lectures designed to introduce the role of Medical Directors and Centers for Medicare and Medicaid regulations pertaining to skilled nursing facilities. Information will also be provided on how to pursue Certification for Medical Directors (CMD).
Clinical and Quality Improvement Research: The program has a 4-week research requirement. The first week consists of structured curriculum to introduce concepts in Quality Improvement research and expose fellows to ongoing projects which they may choose to join. Fellows will be paired with a faculty mentor to develop and carry out clinical or quality improvement research. Publication of research is not required to successfully graduate from the program. However, we strongly encourage fellows to submit abstracts and present at national conferences, including the American Geriatrics Society annual meeting and PALTC.
Medical Education: Fellows have the opportunity to hone their medical education skills by working with University of Virginia residents and medical students. The level of involvement may vary depending on each fellow’s interests. There are ample opportunities for fellows to lead workshops and develop new curriculum if desired.
The UVA School of Medicine is highly ranked nationally. Students rotate through geriatric medicine in their third year as part of a required ambulatory medicine clerkship. The section also offers a geriatric medicine elective to fourth year medical students. Fellows may precept students in these clerkships and electives across all care settings, including home visits. There are plenty of opportunities for curricular development as well.
Mentorship: Ultimately our faculty are focused on training physicians to become our future colleagues in the world of clinical and academic geriatrics. To this end, the program provides individualized mentorship to each fellow, taking into account their professional and personal goals.
Professional Networking: Fellows will have dedicated time and funding to attend national meetings, including the Post-acute and Long Term Care (PALTC) annual meeting and the American Geriatrics Society (AGS) annual meeting. In addition, the program strongly encourages and supports fellows in applying for and attending the AMDA Futures Program.