Rotation Details
Anatomic Pathology
Residents rotate through Surgical pathology on a four-day cycle, with one resident covering the responsibilities for each day (4 residents on service each rotation). The rotation is structured with a hybrid subspeciality sign-out model, with residents rotating through services enriched for the following subspecialties for a week at a time:
- GI/GU
- GYN/Breast
- ENT/Thoracic
- Soft Tissue/Perinatal/Pediatric/Transplant
Residents sign-out the majority of the resection specimens that they gross to provide continuity of care and have daily case caps stratified by their PGY year to preserve education time and ensure their workload is manageable. Although each subspecialty service primarily includes cases from its designated organ systems, depending upon the daily case volume services may be enriched for common “bread and butter” specimens—such as colon polyps and benign hysterectomies—providing a general sign-out experience within the hybrid subspecialty model.
Day 1 – Frozens: Residents are responsible for sectioning specimens for intraoperative evaluation and communicating with surgeons. Histotechnologists assist with processing the slides. First year residents are on shift from 7:30 AM (operating room start time) until 9:30 PM for their first few rotations on this service. Upper level residents cover call after 9:30 PM on the weekdays and after 5:30 PM on Saturday. Later in the year, all residents cover frozen call from 7:30 AM the day of until 7:30 AM the next day. All residents are responsible for communicating the results to the surgeon and documenting the diagnosis.
Day 2 – Grossing: Grossing is the most rigorous part of surgical pathology. On average, residents gross from 9:00 AM to between 6:00 and 7 PM, with an 8 PM evening cap. Additionally, they gross one Saturday per block; a PA is typically present for Saturday grossing, and on the rare occasions that PA do not staff the weekend a junior residents will have upper-level support for Saturday grossing. Residents are responsible for grossing or triaging specimens that are accessioned before 3:00 PM. Specimens that arrive between 3:00 PM and 6:00 PM are triaged for the following day by the Frozens resident. Residents often gross the more complex specimens while support staff cover the biopsy and many simple resection specimens. There are 3.5 full-time dedicated Pathology Assistants who help with a variety of activities in the gross room.
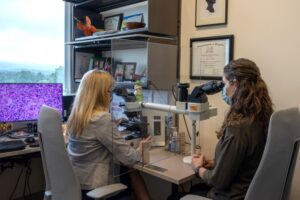
Day 3 & 4 –Sign-out: Slides for resection cases are available in the afternoon on Day 2 and Day 3: the day before a resident sits with an attending for the case’s sign-out. Biopsy slides are available by 7:30 AM on Day 3 and Day 4: the same day a resident sits with an attending for the case’s sign-out.
Sign-out with an attending begins around 10:00 AM each day. Some residents elect to previewing their resections the preceding afternoon/evening, while others prefer to preview early in morning before sign-out. Most do a combination of both to balance their workload and maximize their education. First year residents are not expected to comprehensively preview all of the slides; the purpose of previewing for new first year residents is to review interesting or complex cases in depth, gather paperwork that may be needed for specific cases, and become familiar with the patient’s clinical history. As they gain diagnostic and operational skills, more comprehensive case preview is expected.
After any sign-out, the resident is responsible for dictating the final report, ordering stains/sections, reviewing billing codes, and contacting the patient care team with any urgent results. At the end of Day 4, the resident is also expected to review the operating room schedule for the next day (Day 1 in the four-day cycle) in order to prepare for potential frozen section specimens. On average, most residents are finished with Day 4 by 6:00 PM.
 The autopsy rotation will be staffed by 1-2 residents. First year residents will be paired with an upper level resident for their first rotation. Residents are responsible for verifying consent, communicating with the ordering physician about the decedent’s clinical history, performing the autopsy, reviewing the gross and microscopic findings with the attending, and writing the final report. Most autopsy cases are presented at the biweekly autopsy conferences on Thursday mornings and neuroanatomical examinations are performed on Thursday mornings. Autopsy technicians perform eviscerations, although residents are required to learn how to eviscerate in preparation for their forensic pathology rotation. Any of our pathology assistants can assist with organ dissection as needed. Each year approximately 250 autopsies are performed at the University of Virginia. Residents average 30 – 40 hospital autopsies and another 10 – 20 autopsies during their medical examiner rotation by the end of their training. Autopsies are not performed on Saturdays except for emergencies, so call is covered by the resident on weekend surgical pathology coverage.
The autopsy rotation will be staffed by 1-2 residents. First year residents will be paired with an upper level resident for their first rotation. Residents are responsible for verifying consent, communicating with the ordering physician about the decedent’s clinical history, performing the autopsy, reviewing the gross and microscopic findings with the attending, and writing the final report. Most autopsy cases are presented at the biweekly autopsy conferences on Thursday mornings and neuroanatomical examinations are performed on Thursday mornings. Autopsy technicians perform eviscerations, although residents are required to learn how to eviscerate in preparation for their forensic pathology rotation. Any of our pathology assistants can assist with organ dissection as needed. Each year approximately 250 autopsies are performed at the University of Virginia. Residents average 30 – 40 hospital autopsies and another 10 – 20 autopsies during their medical examiner rotation by the end of their training. Autopsies are not performed on Saturdays except for emergencies, so call is covered by the resident on weekend surgical pathology coverage.
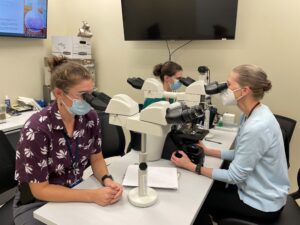 Residents work closely with the UVA hematopathology fellows to run our busy hematopathology service. Daily responsibilities include review of peripheral blood smears and select body fluids (wet-heme signout) with an attending, previewing in-house bone marrows and lymph node/tissues, interpreting flow cytometry results, and a main sign out to review in-house cases and flow cytometry with an attending. There are two multi-headed microscopes dedicated to hematopathology sign-out. There is a weekly hematopathology interesting case conference and journal club. Residents have the opportunity to attend a weekly meeting to discuss results of pertinent corresponding molecular and genetic studies and are invited to attend weekly tumor boards (adult heme-onc and pediatric heme-onc). Residents interested in hematopathology can elect to participate in our 2 week flow cytometry elective and/or can create an elective to rotate on the consult hematopathology service.
Residents work closely with the UVA hematopathology fellows to run our busy hematopathology service. Daily responsibilities include review of peripheral blood smears and select body fluids (wet-heme signout) with an attending, previewing in-house bone marrows and lymph node/tissues, interpreting flow cytometry results, and a main sign out to review in-house cases and flow cytometry with an attending. There are two multi-headed microscopes dedicated to hematopathology sign-out. There is a weekly hematopathology interesting case conference and journal club. Residents have the opportunity to attend a weekly meeting to discuss results of pertinent corresponding molecular and genetic studies and are invited to attend weekly tumor boards (adult heme-onc and pediatric heme-onc). Residents interested in hematopathology can elect to participate in our 2 week flow cytometry elective and/or can create an elective to rotate on the consult hematopathology service.
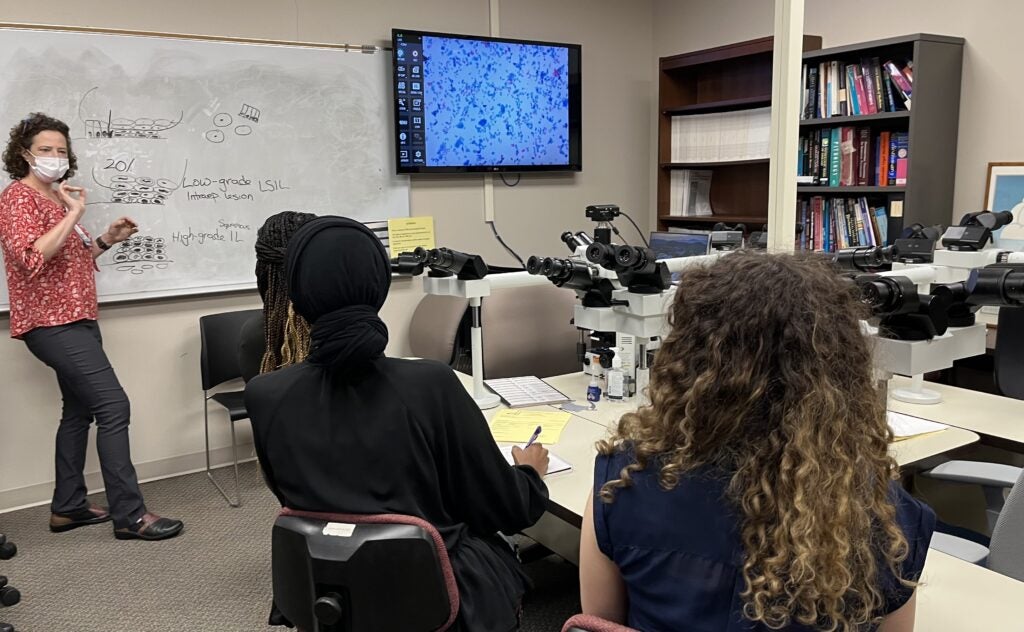
 Residents on the cytology service complete a variety of activities that fluctuate on a daily basis. Generally, residents preview cytology cases, participate in fine needle aspiration procedures, assist with on-site assessments and preliminary diagnoses, and attend daily sign-out. First year residents are encouraged to perform fine needle aspirations on palpable masses and learn how to prepare cytology slides. Highlights of this rotation include interacting with patients, performing procedures, and reasonable working hours. Residents also have the option to spend a few mornings in the histology lab learning how to embed tissue, prepare slides and process stains.
Residents on the cytology service complete a variety of activities that fluctuate on a daily basis. Generally, residents preview cytology cases, participate in fine needle aspiration procedures, assist with on-site assessments and preliminary diagnoses, and attend daily sign-out. First year residents are encouraged to perform fine needle aspirations on palpable masses and learn how to prepare cytology slides. Highlights of this rotation include interacting with patients, performing procedures, and reasonable working hours. Residents also have the option to spend a few mornings in the histology lab learning how to embed tissue, prepare slides and process stains.

Dermatopathology rotations provide the trainees with exposures to a wide breadth of dermatologic diseases. We teach the trainees to exercise the clinicopathologic correlation for inflammatory dermatoses. We offer the opportunity to learn the direct immunofluorescence study in the immunobullous diseases and molecular signatures of unusual melanocytic tumors.
Residents participate in all activities of the diagnostic service of the Division of Neuropathology, which includes the examination of brain smears, frozen sections, and permanent sections of neurosurgical specimens, as well as the gross and microscopic examination of brains obtained from the autopsy material. Consultation case materials submitted from outside centers are also part of the routine evaluation. Residents essentially function as fellows in studying first-hand the neuropathological material under the guidance and supervision of a Neuropathology Fellow and faculty member.
Residents also participate in all clinical and teaching conferences of the division including Neuro-Oncology Tumor Board, Combined Neuropathology Conference, Neuroradiology Rounds, Neuromuscular Conference, Pituitary Conference, Neuropathology Journal Club, etc. Projects in clinicopathologic correlation and/or experimental Neuropathology may also be possible during this rotation.
 Third year residents complete their forensic rotation in one of the four medical examiner offices of Virginia: Central district (Richmond, VA – 70 miles from Charlottesville), Northern District (Manassas, VA – 80 miles from Charlottesville), Tidewater District (Norfolk,VA – 160 miles from Charlottesville), or Western District (Roanoke, 120 miles from Charlottesville). Residents can elect to either commute or relocate for the four-week rotation. Mileage reimbursement or a housing allowance is provided up to $1,200. During the rotation, residents perform autopsies (including eviscerations), visit crime scenes, and contribute to the legal aspects of cases. Work hours are usually from 8:00 AM until 4:00 PM. Most residents average 10-20 cases during this rotation, ten of which can be applied to ACGME board requirements.
Third year residents complete their forensic rotation in one of the four medical examiner offices of Virginia: Central district (Richmond, VA – 70 miles from Charlottesville), Northern District (Manassas, VA – 80 miles from Charlottesville), Tidewater District (Norfolk,VA – 160 miles from Charlottesville), or Western District (Roanoke, 120 miles from Charlottesville). Residents can elect to either commute or relocate for the four-week rotation. Mileage reimbursement or a housing allowance is provided up to $1,200. During the rotation, residents perform autopsies (including eviscerations), visit crime scenes, and contribute to the legal aspects of cases. Work hours are usually from 8:00 AM until 4:00 PM. Most residents average 10-20 cases during this rotation, ten of which can be applied to ACGME board requirements.
On our “Inside-Outside (IO)” rotation, upper level residents work alongside faculty to review cases for patients who have received diagnoses elsewhere but are coming to UVA for care: this service provides a critical quality assurance mechanism for our patients, and allows trainees to encounter a high volume of material enriched for interesting diagnoses. On Trues, upper level residents manage directed consults that run the full gamut of surgical pathology subspecialties, with particular enrichment for gastrointestinal, head and neck, soft tissue, gynecologic, and breast neoplasia. They sign these cases out 1:1 with expert faculty, and hone their communication skills by calling back diagnoses the submitting pathologists.
Clinical Pathology
 Typically two residents at a time are responsible for the daily oversight of the active blood bank and transfusion medicine service. Residents follow multiple complicated patients on a daily basis, assessing transfusion needs and working closely with the clinical teams to optimize blood product utilization. Responsibilities include serologic antibody identification, platelet triage, clinical team consultations, transfusion reaction work ups, hospital-wide product utilization reviews, and preparation for daily rounds with the Blood Bank attendings. Residents are exposed to multiple facets of transfusion medicine. New residents are introduced to the service with a practical training experience with our senior techs.
Typically two residents at a time are responsible for the daily oversight of the active blood bank and transfusion medicine service. Residents follow multiple complicated patients on a daily basis, assessing transfusion needs and working closely with the clinical teams to optimize blood product utilization. Responsibilities include serologic antibody identification, platelet triage, clinical team consultations, transfusion reaction work ups, hospital-wide product utilization reviews, and preparation for daily rounds with the Blood Bank attendings. Residents are exposed to multiple facets of transfusion medicine. New residents are introduced to the service with a practical training experience with our senior techs.
While on Chemistry, second year residents are charged with responding to inquiries regarding available laboratory tests, data interpretation, and testing results. Residents play a major role in assisting clinical teams in appropriate test selection for their patients and are first responders to issues arising in or related to the clinical laboratory. Residents get extensive training in quality measures and lab management approaches, including both statistical and financial considerations, and pursue opportunities for bench work and tech time. Weekly obligations include QC review, laboratory rounds, endocrine conference with the clinical teams, and a call review conference with chemistry faculty and fellows.
 This experience includes sign-outs with coagulation lab faculty. UVA offers a broad spectrum of general and special coagulation assays, which require extensive and sophisticated interpretation and reporting. UVA is a certified ECMO center, so residents have a unique opportunity to learn about the specialized protocols and coagulation monitoring required for these very ill patients.
This experience includes sign-outs with coagulation lab faculty. UVA offers a broad spectrum of general and special coagulation assays, which require extensive and sophisticated interpretation and reporting. UVA is a certified ECMO center, so residents have a unique opportunity to learn about the specialized protocols and coagulation monitoring required for these very ill patients.
 This rotation generally carries no more than one resident at a time and includes both ample tech time in the lab as well as daily rounds with both microbiology and infectious disease faculty. The resident is expected to carry the pager, responding to all microbiology-related inquiries from the clinical teams.
This rotation generally carries no more than one resident at a time and includes both ample tech time in the lab as well as daily rounds with both microbiology and infectious disease faculty. The resident is expected to carry the pager, responding to all microbiology-related inquiries from the clinical teams.
 Molecular genetics is a busy service with a rapidly expanding menu of genetic tests and panels. Typically a second and/or fourth year resident runs the service and is responsible for specimen evaluation and data interpretation on multiple platforms, including next generation sequencing, pyrosequencing, real-time PCR, and capillary electrophoresis. The residents investigate and coordinate send-out requests for molecular studies not available at UVA. The rotation encompasses constitutional and cancer genetics as well as cutting-edge genomics approaches to diagnosis. Residents have robust involvement in chromosomal microarrays, fluorescence in situ hybridization (FISH), and conventional karyotype analysis. Residents attend daily rounds for molecular and cytogenetics sign-outs, participate in a biweekly pediatric genetics conference and in a weekly hematology/oncology tumor board, and act as liaison between the labs and the clinical teams.
Molecular genetics is a busy service with a rapidly expanding menu of genetic tests and panels. Typically a second and/or fourth year resident runs the service and is responsible for specimen evaluation and data interpretation on multiple platforms, including next generation sequencing, pyrosequencing, real-time PCR, and capillary electrophoresis. The residents investigate and coordinate send-out requests for molecular studies not available at UVA. The rotation encompasses constitutional and cancer genetics as well as cutting-edge genomics approaches to diagnosis. Residents have robust involvement in chromosomal microarrays, fluorescence in situ hybridization (FISH), and conventional karyotype analysis. Residents attend daily rounds for molecular and cytogenetics sign-outs, participate in a biweekly pediatric genetics conference and in a weekly hematology/oncology tumor board, and act as liaison between the labs and the clinical teams.

