Hemangioblastoma
Hemangioblastoma Research and Outcomes Data from UVA Gamma Knife
The gold standard treatment for hemangioblastomas is the surgical resection of the solid component of the tumor. It is not necessary to resect, if present, the cystic portion of the tumor. Similarly with Gamma surgery we have treated only the solid portion of these tumors. The results of 11 of our patients with hemangioblastomas have been reported. Four of these patients had von Hippel-Lindau disease. These patients were followed for an average of 27 months and were treated with a maximum dose of 28 to 60Gy and a peripheral dose of 11 to 20Gy. The usual course was either a decrease in the size of the solid component (7/10) of the tumor or no change (3/10). One patient with a history of multiple hemangioblastomas and extirpations had dramatic tumor shrinkage of a pineal region hemangioblastoma and continues to do well more than 9 years after her Gamma surgery.
Pre / Post Gamma Knife
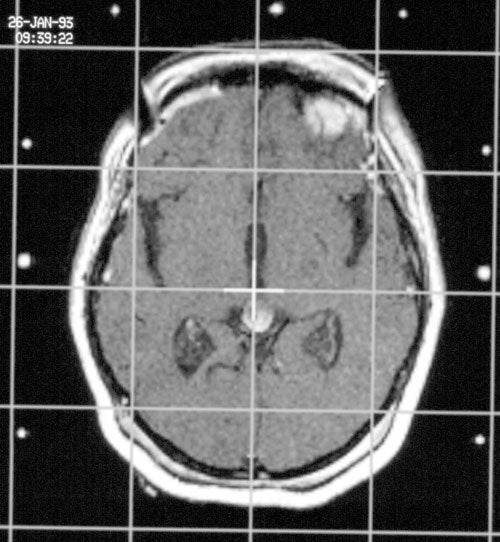
Pre Gamma Knife
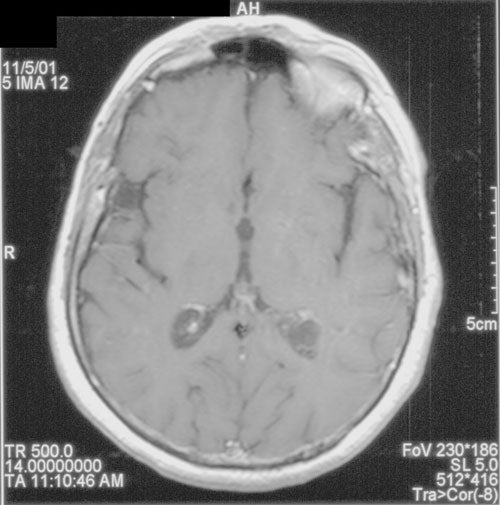
Post Gamma Knife
It was not uncommon however for the cystic portion of the tumor to grow larger regardless of the behavior of the solid portion. During the follow-up of these patients four patients required open surgery for relief of expanding cysts and two for unresponding solid tumors.
Although several patients responded well, the high incidence of second, open procedures indicates that the microsurgical removal of hemangioblastomas is in most cases the initial procedure of choice.
Hemangiopericytomas
Intracranial hemangiopericytomas are richly vascular, rapidly growing mesenchymal neoplasms. They have a predilection for both local and distant central nervous system recurrence and an increased tendency to metastasize. Although surgical resection is the gold standard for these tumors, the high recurrence rate and operative mortality, Gamma surgery presents an attractive option for treatment of hemangiopericytomas.
A retrospective analysis of 12 patients treated at the University of Virginia with 15 separate intracranial hemangiopericytomas revealed reasonable short-term, local tumor control with 9 tumors decreasing in volume and 3 remaining stable. However, 4 of the 9 tumors that initially shrank later progressed at a mean of 22 months post-radiosurgery. In a similar fashion, the University of Pittsburgh group found a local tumor control rate of 76% at a mean follow-up of 31 months post-radiosurgery; the 5 year survival rate was 100%. However, radiosurgery did not seem to offer protection against the development of intra- or extracranial metastases. Gamma knife surgery appears to offer effective acceptable short-term local tumor control for these otherwise untreatable tumors.
Click here for information about brain tumor Causes, Symptoms, Diagnosis and more treatment options.
