Minimally Invasive Spine Surgery
As in various surgical subspecialties using small surgical corridors to approach pathologies, the development of minimally invasive approaches to the spine has revolutionized contemporary spine surgeries. Modern minimally invasive surgery (MIS) techniques allow spine surgeons to achieve the same goals of open surgery while minimize the collateral damage associated with the open approaches. Using MIS techniques, surgeons are able to avoid a long incision and extensive muscle dissection. Reducing tissue injuries can result in decreased blood loss, reduced postoperative pain, shortened hospital stay and expedited recovery. Several laboratory, imaging and biomechanical studies have shown that MIS approaches reduce paraspinal muscle atrophy and allow greater preservation of normal spinal motion.
Spine surgery is recommended when a period of nonsurgical treatment such as medications, physical therapy, or epidural steroid injections cannot provide adequate relief of neck or back painful symptoms. Indications of minimally invasive spine surgery include:
Chun-Po Yen, MD
Information on this page was compiled by our primary minimally invasive spine surgeon Dr. Chun-Po Yen.
- Herniated disc (cervical disc, thoracic disc, lumbar disc)
- Spinal stenosis
- Spondylolisthesis
- Degenerative spinal disease
- Spine deformity such as scoliosis or sagittal malalignment (kyphosis)
- Spinal fracture
- Spinal infection
- Spinal tumor
For above mentioned spine problems, some MIS procedures including decompression, instrumentation, fusion, correction of deformity or a combination of them are employed to treat the spine diseases.
Chun-Po Yen, MD
Information on this page was compiled by our primary minimally invasive spine surgeon Dr. Chun-Po Yen.
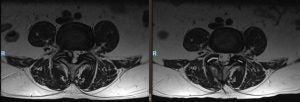
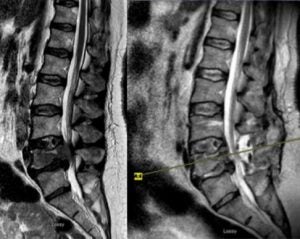
Lumbar disc herniation
A herniated or bulging disc that pinches a nerve can cause leg pain, numbness, or weakness. Using a muscle splitting percutaneous technique, a tubular retractor can be placed through a less than 1-inch incision and the natural muscular planes to reach the spinal column. A small bony resection called laminectomy is performed to allow the surgeons to reach the spinal canal, carefully retract the nerve, and remove the herniated disc. This approach avoids a big incision or muscle stripping associated with traditional open surgery. The procedure is usually performed in an outpatient setting.
Herniated Disc - Patient Education
Thoracic disc herniation
 Surgery to remove thoracic disc herniation is more challenging compared to that for lumbar disc herniation as spinal cord is not amenable to manipulation. Posterior approach to remove thoracic disc carries a high risk of morbidities and have been largely abandoned. A posterolateral approach requiring extensive tissue dissection or a large thoracotomy requiring deflation of lung are alternatives but usually lead to significant postoperative pain and lengthy recovery. A mini-open lateral thoracotomy and retropleural microdiscectomy employ a 6-7 cm skin incision and limited rib resection to safely remove the thoracic herniated disc without violating the pleural cavity. Instrumentation and fusion are not required and the rate of postoperative complication is low.
Surgery to remove thoracic disc herniation is more challenging compared to that for lumbar disc herniation as spinal cord is not amenable to manipulation. Posterior approach to remove thoracic disc carries a high risk of morbidities and have been largely abandoned. A posterolateral approach requiring extensive tissue dissection or a large thoracotomy requiring deflation of lung are alternatives but usually lead to significant postoperative pain and lengthy recovery. A mini-open lateral thoracotomy and retropleural microdiscectomy employ a 6-7 cm skin incision and limited rib resection to safely remove the thoracic herniated disc without violating the pleural cavity. Instrumentation and fusion are not required and the rate of postoperative complication is low.
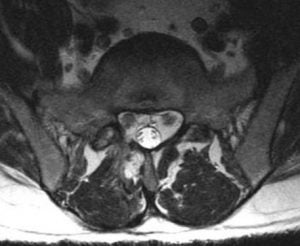
Spinal stenosis
Spinal stenosis is abnormal narrowing of the vertebral column due to disc degeneration, thickened ligament, or synovial cyst that results in pressure on spinal cord or nerve roots. Patients with spinal stenosis usually present with so called “neurogenic claudication”. They are not able to stay upright ambulating; tend to lean on a shopping cart; or require multiple breaks sitting or bending down to be able to ambulate for a longer distance. Surgical treatment is to remove the posterior bony structure and thickened ligament to widen the spinal canal (laminectomy) or nerve root tunnel (foraminotomy).
 Compared to traditional open surgery that stripping the paraspinal muscles and weakened the posterior tension band to reach the spine. A bilateral decompression can be performed via a unilateral tubular retractor technique through a small incision. Surgeons are able to preserve posterior tension band to prevent post-laminectomy flat back syndrome. The procedure is in general performed in an outpatient setting.
Compared to traditional open surgery that stripping the paraspinal muscles and weakened the posterior tension band to reach the spine. A bilateral decompression can be performed via a unilateral tubular retractor technique through a small incision. Surgeons are able to preserve posterior tension band to prevent post-laminectomy flat back syndrome. The procedure is in general performed in an outpatient setting.
Degenerative spinal disease
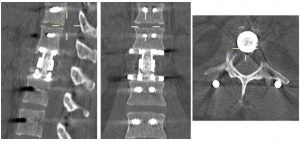
Patients with advanced degenerative spinal degeneration have severe disc degeneration, canal or nerve root tunnel stenosis resulting in low back pain, leg pain, numbness, weakness or difficulty ambulating. Patients with multilevel degenerative disease might require decompression, instrumentation, and fusion. Traditional open surgery requires extensive muscle stripping, bony resection to gain access the disc spaces and placement of rods and screws. MIS procedures use small corridors to access the disc spaces through small posterior or lateral incisions to perform discectomy and interbody fusion. The rods and screws can be placed in a percutaneous fashion using multiple small skin incisions.
MIS transforaminal lumbar interbody fusion (TLIF)
TLIF is one of the most common performed fusion procedures. Instead of a wide skin opening, spine surgeons can now use a specially designed retractor to remove lamina. The surgeons can then reach the disc space to remove the degenerative disc and place a cage and bone graft to restore the disc space and promote fusion.
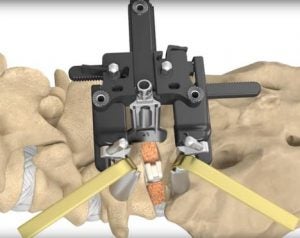


Extreme lateral lumbar interbody fusion (XLIF)
The extreme lateral lumbar interbody fusion is a novel minimally invasive procedure that provides a surgical corridor to the anterior thoracic or lumbar spine for fusion. The patient is placed in a lateral decubitus position. A small incision and meticulous dissection allow placement of a series of dilators and retractor to safely reach the latera aspect of spine with the guidance of neuromonitoring and x rays. Once reaching the disc space, discectomy and interbody fusion can be performed and distraction of the disc space allowing effective decompression of pinched nerve without direct bony removal.



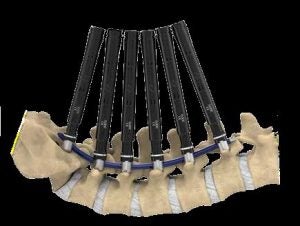
Percutaneous screws
Spinal instrumentation such as screws and rods are used to stabilize spinal column to allow operated spine segment to fuse. It is also used to correct the spinal deformity. Traditional approach for placement of screws and rods requires a long incision and extensive detachment of muscles from spine column. MIS techniques allow percutaneous (through the skin) placement of screws and rods using small skin incisions without cutting the underlying muscles or ligaments. With the guidance of x rays or navigation system, surgeons accurately place the screws into vertebrae along the desired path. There screws have temporary extenders that extend outside of the skin and subsequently removed after assisting to guide passage to rods to connect and secure the screws.


Spinal deformity
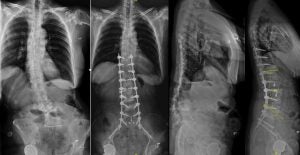 Spinal deformity includes scoliosis and sagittal malalignment. Traditional open surgery requires large exposure for decompression, instrumentation and fusion. MIS approach utilize a lateral approach to restore the disc height to achieve decompression. A large foot print cage spanning across the hardest part of vertebral bodies avoids the cage subsidence, which is especially beneficial for patients with osteopenia or osteoporosis. Long segment pedicle screw fixation can be performed in a percutaneous fashion. Computer guided rod bending system allows efficient rod contouring and placement even in cases needing long segment instrumentation. Preoperative and intraoperative planning computer program help surgeons create a preoperative plan and execute the desired correction of the deformity and realignment of spine curvature. These tools are critical for spine surgeons to achieve good outcomes in patients with degenerative scoliosis or sagittal malalignment.
Spinal deformity includes scoliosis and sagittal malalignment. Traditional open surgery requires large exposure for decompression, instrumentation and fusion. MIS approach utilize a lateral approach to restore the disc height to achieve decompression. A large foot print cage spanning across the hardest part of vertebral bodies avoids the cage subsidence, which is especially beneficial for patients with osteopenia or osteoporosis. Long segment pedicle screw fixation can be performed in a percutaneous fashion. Computer guided rod bending system allows efficient rod contouring and placement even in cases needing long segment instrumentation. Preoperative and intraoperative planning computer program help surgeons create a preoperative plan and execute the desired correction of the deformity and realignment of spine curvature. These tools are critical for spine surgeons to achieve good outcomes in patients with degenerative scoliosis or sagittal malalignment.
Spinal trauma
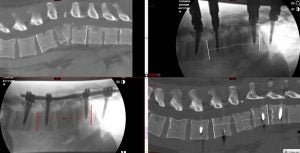 In selected patients, the spine fracture can be stabilized and fixed with rods and screws using MIS technique. Special device can be used to correct the spinal deformity associated with spinal fracture and restore spinal alignment. Percutaneous pedicle screws are often used to maintain spine alignment after correction and provide rigid support for bone healing.
In selected patients, the spine fracture can be stabilized and fixed with rods and screws using MIS technique. Special device can be used to correct the spinal deformity associated with spinal fracture and restore spinal alignment. Percutaneous pedicle screws are often used to maintain spine alignment after correction and provide rigid support for bone healing.
Spinal infection
Infection of disc (diskitis) or vertebral body (osteomyelitis) can cause back pain, leg pain, or neurologic deficits. Patients refractory to antibiotic treatment or those developed spinal instability or deformities require surgery. MIS lateral approach using a small incision can reach the thoracic or lumbar spine to remove the infected tissues. The spinal column can be restored with the new expandable cage technology and stabilized with percutaneous screws and rods.



Spinal tumor
Spinal metastases account for the majority of spinal tumors. With the advance of chemotherapy or target therapy, the cancer patients are enjoying longer survival while more patients are diagnosed with spinal metastases. Patients with metastatic tumors to spine were relegated to palliative radiotherapy in the past. Advance of surgical technique and radiosurgery has provided cancer patients a new treatment option. MIS procedure allow aggressive removal of tumor. Even in patients with extensive metastatic disease, surgeons can safely separate the tumor from critical neural tissues to allow radiation oncologists to deliver high dose focused radiation to control tumor growth. Various minimally invasive techniques such as mini open decompression, corpectomy and percutaneous fixation allow spine surgeons to remove the tumor with small incisions and effectively separate the tumor from nerves and spinal cord. A short recovery period and expedited wound healing allow the radiation oncologists to start radiation without delay.

Limitations
As with any new surgical technique, there is a learning curve to become proficient in MIS procedures. Additionally, not all the patients are candidates for this type of procedure. UVA spine center is staffed with experienced spine surgeons providing up to date MIS techniques to treat various spinal diseases.
For more information, email or call us at:
Evan Turnbull, PA
Lois Osteen, scheduler/assistant
434-297-7462