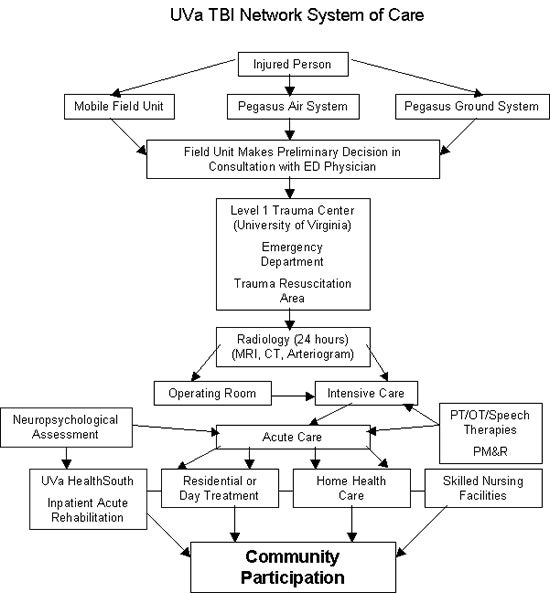
TBI Continuum of Care
This page describes how patients are cared for throughout the UVa Traumatic Brain Injury (TBI) Network, as shown in this diagram. The sheer number of specialties that touch a patient’s life may seem confusing and daunting to patient and family. We provide the best care possible, thanks to our team of highly trained professionals, and we coordinate the care across all specialties. It is also our objective to make the patient’s transitions and progress through the continuum of care as smooth as possible.
Emergency Medical System
The regional EMS organization serves the eight counties surrounding the UVa Health System-a region of about 3,400 square miles-with 25 Advanced Life Support squads, 19 volunteer fire companies and the Shenandoah National Park Medic program. An area of roughly twice that size actively utilizes UVa Health System as a referral destination for trauma and neurotrauma patients. This includes large areas of the Shenandoah Valley and the I-81 corridor, southern and southwest Virginia, and many counties of West Virginia.
Emergency Department
Physicians are notified of an incoming patient and interact with the EMS units by radio. The emergency physicians contact trauma and neurotrauma teams, who call in additional personnel and resources before the patient arrives. The emergency medicine attending physician and a senior emergency resident physician are responsible for initial assessment, airway interventions and stabilizing procedures. The Director of Neurological Emergency Medicine sees most patients with TBI. The typical team response to a “Neurotrauma Alert” includes physicians from Neurosurgery, Trauma Surgery, Emergency Medicine and Anesthesiology, as well as respiratory therapy staff, radiology staff and other professionals.
Neurosurgical Care
Our neurosurgeons perform about 2,500 major emergency and elective operations each year. Procedures for TBI patients include emergency craniotomies, intracranial pressure (ICP) monitoring, shunt placement, ventriculostomy, decompressive craniectomy, evacuation of intra- and extracranial hematomas, complex reconstruction of the skull and skull base, and treatment of cerebrospinal fluid (CSF) fistulae.
Intensive Care Units
Intensive care for TBI is structured in the following way at UVa Health System. All adult patients with multiple injuries are admitted to the Surgical Trauma ICU (STICU) under the care of the trauma director and trauma team. All patients are closely monitored by neurosurgeons who consult on their cases.
After being thoroughly assessed for other life-threatening injuries and cleared by the trauma service, patients with isolated head injuries are admitted to the Nerancy Neuro Intensive Care Unit (NNICU). Patients in the NNICU are either critically ill or have just come from complex brain or spine surgery.
Pediatric patients with TBI are admitted to the Pediatric ICU (PICU). The overall volume in the PICU is about 800 to 900 admissions per year with 125 to 150 trauma admissions per year. About one third of the trauma patients have significant brain injury. Care of pediatric patients with multiple injuries is collaborative. Professionals from the Critical Care, Pediatric Surgery and Neurosurgery services all contribute their insights to an ideal treatment plan.
A TBI management protocol for ICUs has been in place since July 1997. All ICUs have 24-hour housestaff coverage, and attending physicians are board-certified in critical care. All units are covered 24 hours a day, seven days a week by respiratory therapy staff, laboratory staff for arterial blood gases and stat laboratory studies, and emergency staff for neuroimaging and X-rays. Rehabilitation therapies, including speech pathology, physical therapy and occupational therapy, begin while the patient is still in the ICU.
Patients who have been stabilized and no longer require the intense level of care provided in the ICU move to another bed in the “step-down” unit, where the level of care still exceeds that provided in a traditional inpatient setting. Patients may move from the NNICU to the Spine Unit or Stroke Unit.
Since 1997, a coordinated effort has been made to use the guidelines for brain injury management published by the American Academy of Neurological Surgeons as a template for brain injury care at UVa. These guidelines were adapted to include the extensive, coordinated experience at UVa. Our outcomes equal or exceed the best outcomes reported in the literature to this date.
Rehabilitation
At the acute level, UVA provides rehabilitation in a safe, structured, secure environment with a 24-hour Rehabilitation Companion assigned on admission. Immediate assessments and treatments initiated by psychiatry, rehabilitation nursing, neuropsychology, occupational therapy, physical therapy, and speech-language pathology are delivered. The team first assesses the patient within 48 hours of admission. Because the family is crucial to recovery, the initial team/family conference is held upon admission.
One-on-one therapies offer the following elements every day:
- Gait training
- Respiratory care
- Spasticity management
- Positioning and orthotics
- Sensory stimulation
- Swallowing
- Communications
- Self-care
- Cognition
- Functional mobility
- Pharmacological intervention
- Reality counseling
- Support services with the family
As the patient progresses in the acute rehabilitation phase, we add other therapies.
Adult patients may receive additional therapy at our rehabilitation hospital, UVa-HealthSouth. Children receive the full range of therapy at the Kluge Children’s Rehabilitation Center.
Neuropsychology
Neuropsychology as a clinical specialty has evolved from being a consultative service to being more actively involved in multidisciplinary treatment teams, with faculty from several clinical departments.
The University of Virginia’s Neuropsychologists specialize in assessing brain-behavior relationships, and cognitive and behavioral strengths and weaknesses. Neuropsychological assessments are standardized, objective tests that quantify neurocognitive deficits and compare each patient’s performance to a general population of same-age peers. These evaluations also include a clinical interview conducted by a clinical neuropsychologist and an objective personality measure to identify psychological distress that might be contributing to the patient’s symptoms.
For a TBI patient, neuropsychology often is involved at the inpatient level. The work consists of brief patient assessments, family education, and developing behavior-management protocols. Patients may be seen by the neuropsychologist at the six-week follow-up visit, and also may be referred to neuropsychology later in recovery depending on patient needs and function.
Community Re-integration
The rehabilitation process does not end when the individual is discharged from the acute rehabilitation center. Rehabilitation continues through a wide range of outpatient, day services, and home care activities. The UVa TBI Network program works in cooperation with the UVa Home Health Care Services network.
UVa-HealthSouth has a Neuro Day Treatment Program in the NeuroRecovery Center for TBI patients. The NeuroRecovery Center works to improve the quality of life and functional independence of people with neurologic disorders by offering exceptional rehabilitation care and management. The Day Treatment program offers comprehensive outpatient treatment for people with complex neurorehabilitative needs. A multidisciplinary treatment team performs an initial assessment before enrollment. The team then designs an individualized program that will achieve the best recovery. Physicians and therapists who oversee the individual’s rehabilitative care review their patient’s progress each week. At the end of each day, patients return home to the care of family members.
The program is geared toward integration back into the community. There are also specialized day clinics for medication review, neurobehavioral problems, substance abuse, and a wide range of complementary medical rehabilitation services. These services include massage therapy, acupuncture, dance and movement therapy, and horticultural therapy.
Linkages and referrals are made to the state vocational and social services administration, as well as to independent living centers and community support programs. There is a close collaboration with the Woodrow Wilson Rehabilitation Center in the Shenandoah Valley, where transitional living programs are available, and where vocational training and career planning is provided. UVa-HealthSouth also provides linkages to the Brain Injury Association of Virginia support groups.
